By Diane Millman, J.D.
National Coalition for Quality Diagnostic Imaging Services (NCQDIS)
On March 26, 2004, the U.S. Centers for Medicare and Medicaid Services (CMS) published the long-awaited phase II of the Stark law regulations in the Federal Register.
The Stark Law refers to a set of laws sponsored by Rep. Fortney "Pete" Stark (D-CA) that prohibit physicians from referring Medicare and Medicaid patients for designated health services (DHS) to entities with which the referring physicians have a financial relationship. However, there are almost 20 exceptions to the Stark statute, and qualifying for several of these exceptions means meeting the law’s definition of a "group practice."
Phase I of the Stark regulations addressed the majority of the issues involved in implementing the federal proscription on physician self-referral. Phase II addresses the remaining issues and responds to public comments.
In general, the phase II regulations attempt to ease the regulatory burden of the Stark Law by broadening its exceptions. Phase II has a 90-day comment period and will take effect 120 days after the date of publication.
The body of Stark II regulations are mind-numbingly complex, and therefore difficult to summarize in a single article. Instead, I'll present a number of the changes that may be of particular significance to the diagnostic imaging industry:
Nuclear medicine
The Stark Law prohibition will not extend to nuclear medicine procedures at this time, but CMS will continue to consider this issue.
Time-sharing an imaging facility
A group or individual practice may time-share a diagnostic imaging facility with another entity if the group or individual practice has an office in the "same building" as the diagnostic imaging facility, and that office is used for the provision of "substantial" services "unrelated to" the provision of the diagnostic imaging services or any other services covered under the Stark Law. This standard has not provided clear guidance to physician and group practices wishing to time-share diagnostic facilities that are not located in the same building as their primary practices.
An individual or group practice may meet the Stark Law requirements related to the location of the DHS services if one of the following three standards is met:
- The referring physician or group has an office that is open to the doctor’s or group’s patients for medical services at least 35 hours per week, and the doctor or one or more other doctors in the group furnishes physician services, some of which are unrelated to DHS, at least 30 hours per week.
- The patient receiving DHS usually receives physician services from the doctor or group, the doctor or group owns or rents an office that is open for medical services at least eight hours per week, and the referring doctor furnishes physician services at that location, including some unrelated to DHS, at least six hours per week.
- The referring doctor is present and orders the DHS during a patient visit on the premises or the referring doctor or another member of the group is present while the DHS is furnished during occupancy of the premises, the location meets the eight-hours-per-week requirement above, and the referring doctor or a member of the group meets the six-hours-per-week requirement above.
Thus, under the Stark II regulations, the physician group need only provide some services unrelated to DHS -- not "substantial" services.
Defining Group Practice
In general, the "in office" ancillary services exception applies only if the group also meets Stark’s definition of a bona fide group practice. The major elements of that definition are unchanged in the phase II rule, but certain aspects are tweaked and clarified -- generally making it somewhat easier for groups to meet the requirements.
A group may now say that its "primary purpose" is to function as a group practice if its current operations are consistent with this purpose and will not be assessed based on the intentions of the founders of the group.
A practice can consist of a "single legal entity" even if it has more than one legal entity; if the multiple entities operate in different states, each of which is contiguous to another; if ownership, governance, and operations of each entity are identical; and if the multiple entities are required by state laws.
The group must still include "two or more physicians;" however, the physicians may be part-time as long as other requirements are met.
Leased physicians can be "members" of the group if they are bona fide employees under Internal Revenue Service rules.
Locum tenens and "on call" physicians can be "members" of the practice for the time they serve the practice.
Groups that fail to meet the "substantially all (75%) services" requirement solely because of the addition of a newly relocated physician joining the group now have a 12-month grace period to come back into compliance with this part of the definition.
The previous requirement for centralized utilization review has been deleted from the "unified business" requirement.
Special rules for compensation based on productivity bonuses and profit sharing can be used for independent contractors and members of a group.
These provisions are "deeming rules" -- not exclusive options for determining that productivity bonuses and profit shares do not relate directly to the volume or value of DHS referrals.
Purchasing DHS from mobile providers
Groups can purchase DHS (including diagnostic imaging services) from mobile providers that they do not own or lease on a full-time basis (i.e. "24/7"), as long as the services are billed without markup under Medicare’s purchased diagnostic services rule.
Per-unit payments
"Per-click" arrangements and other per-unit or per-time payments will not take into account the volume or value of referrals if they are priced at fair market value and if the pricing does not change in response to volume during the term of the arrangement.
Compensation
Phase I stated that employers and entities with which physicians can contract can condition compensation arrangements on requirements to refer to a particular DHS provider or network if certain safeguards are included (patient preference, insurer provider selection, and medical judgment as to best interests of the patient). Phase II retains these provisions while adding two new safeguards:
- The requirement to refer must relate solely to the physician services covered by the employment or contract arrangement.
- The requirement is reasonably necessary to effectuate the legitimate purposes of the compensation relationship.
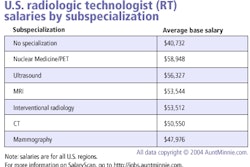
A principle underpinning much of the Stark Law is that compensation arrangements between DHS entities and physicians must be at fair market value, but previous Stark rules provided only general criteria for determining fair market value.
Phase II retains the general criteria and adds to the definition a safe harbor for services personally performed by non-ER physicians if the hourly rate of compensation does not exceed the average of the fiftieth-percentile national compensation figures by specialty in at least four of six specified salary surveys.
For purposes of the salary-survey option, annual income data is to be divided by 2,000 hours to produce an hourly rate. Where the surveys do not include the relevant specialty, the survey data for general practice is to be used. This guideline may be applicable to diagnostic imaging services that provide payment to referring physicians (i.e. nonradiologists) for professional and other services.
An exclusion for radiology by radiologists
The phase II Stark regulations modify the requirements that must be met for a diagnostic imaging center to take advantage of the Stark Law exclusion applicable to radiology services ordered by radiologists. Under current law, to fall outside the scope of the Stark Law, radiologists ordering radiology services must be furnished by, or under the supervision of, a radiologist in accordance with a request for a consultation requested by another physician.
The Stark II regulations make it clear that such supervision may be provided by any member of the radiologist’s group practice and need not be performed by the radiologist to whom the patient is initially referred. CMS reiterates that, for radiology services ordered by a radiologist to fall outside the scope of the Stark Law, the services must be provided under whatever form of supervision is otherwise required for Medicare coverage purposes.
Independent contractors
Independent contractors may be paid on a percentage basis as long as the methodology is established in advance and does not change over the course of the arrangement in any manner that reflects the volume or value of referrals or other business generated by the referring physician.
This change will enable radiologists and other physicians who provide professional services to a hospital, and who also refer Medicare patients to the hospital for inpatient or outpatient hospital services, to be paid by the hospital on a percentage basis. In addition, under the revised regulation, independent-contractor physicians may be paid a bonus based on work that they personally perform.
By Diane Millman, J.D.AuntMinnie.com contributing writer
May 13, 2004
The NCQDIS, based in Washington, DC, is a professional organization that represents more than 2,400 outpatient diagnostic imaging centers and departments in the U.S. Through affiliated professional societies, the NCQDIS message reaches over 150,000 centers and professionals involved in providing diagnostic imaging services. For more information about NCQDIS, visit http://www.ncqdis.org/.
Related Reading
Due diligence builds imaging center muscle, December 19, 2002
Final rules bar doctors from profiting on Medicare "self-referrals", January 4, 2001
U.S. fraud and abuse rules create a minefield for imaging vendors, August 31, 2000
Copyright © 2004 NCQDIS