Researchers have learned more about pairing blood plasma testing and medical imaging over time to understand the Alzheimer's disease process, according to research presented December 2 at RSNA 2025.
The study is among the first evaluating the potential impact of obesity on blood-based biomarkers (tau and amyloid) associated with Alzheimer's, according to lead author Soheil Mohammadi, MD, and colleagues at the Mallinckrodt Institute of Radiology (MIR) at Washington University School of Medicine in St. Louis, MO.
Beta-amyloid plaque deposits and tau protein neurofibrillary tangles are considered two hallmarks of Alzheimer's disease. The impact of obesity on trajectories of amyloid burden and corresponding changes in tau is an important consideration for clinical practice, according to Mohammadi.
The MIR research team accessed five years of data on 407 participants from the Alzheimer’s Disease Neuroimaging Initiative (ADNI), including information from amyloid PET scans and blood plasma samples. Using six commercial laboratory tests, they analyzed plasma samples for three biomarkers associated with Alzheimer's: phosphorylated tau 217 (p-tau217), neurofilament light chain (NfL), and plasma glial fibrillary acidic protein (GFAP).
They then studied the three-way interaction between the baseline blood biomarkers (BBMs), time, and obesity and validated the biomarkers against the amyloid PET scans.
According to their results, at the baseline cross-sectional level, body mass index (BMI) was not significantly associated with whole-brain amyloid burden. However, participants with baseline obesity did exhibit a "significantly greater rate of amyloid accumulation" over time compared with nonobese individuals, the group noted.
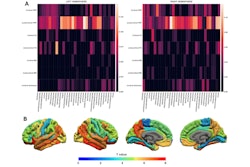
 Axial color scales images of two brains show examples of an amyloid positive scan with a higher centiloid (CL) number and more red colors compared to a normal scan with normal background binding of the amyloid tracer signifying no amyloid plaques.Image and caption courtesy of RSNA.
Axial color scales images of two brains show examples of an amyloid positive scan with a higher centiloid (CL) number and more red colors compared to a normal scan with normal background binding of the amyloid tracer signifying no amyloid plaques.Image and caption courtesy of RSNA.
Comparatively, participants with obesity had a 29% to 95% faster rate of increase in plasma p-tau217 ratio levels. Baseline obesity led to a 24% faster rate of increase in plasma NfL and a 3.7% faster rate of increase in amyloid accumulation, the group reported.
Also, BMI showed no significant correlation with p-tau217 levels as measured by two of the blood plasma tests but had negative associations with the other tests' measurements, according to the group. Furthermore, the study confirmed how blood volume (BV) can affect blood biomarker measurements.
Analysis of the BBMs and PET scan data demonstrated that at baseline, BMI was associated with lower BBMs and reduced whole-brain amyloid burden.
“We believe the reduced BBMs in obese individuals was due to dilution from the higher blood volume,” Mohammadi said in an RSNA statement. “In fact, by relying on the baseline measurements, you could be fooled into thinking that the people with obesity had a lower pathology of Alzheimer’s disease. We need the longitudinal data to fully understand how obesity impacts the development of Alzheimer’s pathology.”
Principal investigator Cyrus Raji, MD, PhD, of the Neuroimaging Labs Research Center at MIR, said the analysis demonstrated that the blood tests were more sensitive than the PET scans in capturing the impact of obesity on Alzheimer’s pathology.
“The fact that we can track the predictive influence of obesity on rising blood biomarkers more sensitively than PET is what astonished me in this study,” Raji noted.
Longitudinal data generation -- repeatedly collecting data from the same group over an extended period -- and mining PET and MRI imaging and laboratory testing data could enable radiologists, other physicians, and healthcare teams to better understand Alzheimer's, the authors said. In addition, the findings could eventually lead to tracking the effects of weight loss drugs on Alzheimer's disease pathology and blood biomarkers, they concluded.