Victims of intimate partner violence with suicidal behavior have certain injury patterns on medical imaging, and radiologists may be the only healthcare providers who can identify subtle injuries and patterns, according to a December 2 presentation at RSNA 2025.
Characterizing the interaction of intimate partner violence and suicidal behavior in radiologic injury patterns may improve screening and facilitate early intervention to better protect vulnerable populations.
To that end, researchers at the Trauma Imaging Research and Innovation Center at Massachusetts General Hospital and Brigham and Women’s Hospital in Boston have studied 1,451 women who reported intimate partner violence to the hospital from 2013 to 2018. Patients reporting intimate partner violence (IPV) are at significantly increased risk of suicidal behavior (SB) and tend to end up at the hospital years before those without.
“As suicide remains a leading cause of death worldwide, our evidence of distinct and overlapping injury patterns with intimate partner violence is an important step towards improving detection and providing timely intervention," said study co-author and Harvard Medical School student Emily Yang, in an RSNA statement.
Radiologists have a unique opportunity to uncover the hidden concerns behind injuries, added senior author Bharti Khurana, MD.
Khurana and colleagues analyzed a total of 151,544 radiology reports, studying the relationship between radiologic injury patterns and suicidal behavior and how they interact to influence healthcare utilization. The group developed four groups: IPV+/SB+ (n = 84), IPV+/SB- (n = 419), IPV-/SB+ (n = 31), and IPV-/SB- (n = 1,207).
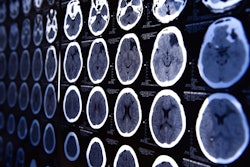
 Head CT of intimate partner violence patient with left-sided parietal subdural hematoma (arrow).Caption and image courtesy of the RSNA.
Head CT of intimate partner violence patient with left-sided parietal subdural hematoma (arrow).Caption and image courtesy of the RSNA.
Suicidal behavior occurred in 16.7% (84 of 503) patients reporting intimate partner violence versus 2.5% (31 of 1,238) patients without a history of intimate partner violence, the group found. Khurana and colleagues also highlighted the following results:
- Intimate partner violence patients with suicidal behavior (IPV+/SB+) suffered more than six times as many head, face, and neck injuries, almost four times as many spinal fractures, three times as many deep injuries, and twice as many upper extremity injuries.
- IPV+/SB+ patients experienced almost twice as many severe injuries and three times as many mild injuries.
- Intimate partner violence had a greater impact on head, face, and neck injuries (3.34 vs. 1.85), whereas suicidal behavior had a greater impact than IPV on the injury rate of upper extremity injuries (1.81 vs. 1.33, p < 0.05).
Also, patients with suicidal behavior and a history of IPV were more likely than other patients to present to the hospital during the night versus during the day and in the ER versus in non-ER settings, according to the group.
Overall, the cooccurrence of IPV and SB showed a synergistic increase in the frequency of injuries across multiple anatomic sites, the authors noted, adding that there is significant potential in understanding suicidal behavior's intersection with IPV.
“By recognizing recurring imaging patterns in patients experiencing intimate partner violence, especially those exhibiting suicidal behavior, we can initiate critical interventions earlier and potentially save lives,” Khurana said.