Congestive Heart Failure
Clinical:
Congestive heart failure (CHF) is a debilitating and common condition affecting 6-10% of the elderly population in developed countries [1]. Approximately 550,000 new cases are diagnosed annually [6]. Heart failure is the leading cause of morbidity, mortality, and hospitalization in patients older than 60 years of age [3]. In North America, the most common cause of CHF is ischemic heart diease (CAD is the underlying etiology for heart failure in 70% of cases [6]) [1]. Left bundle branch block (LBBB) can be found in about 25% of affected patients and has been reported to be associated with increased disease severity and mortality [1]. The long term prognosis for patients with heart failure is poor with a 5-year mortality of 59% for men and 45% for women [2]. The prognosis is generally worse for CHF patients with CAD compared to those without CAD [6]. Approximately 50% of heart failure deaths are caused by ventricular tachycardia [3]. Routine implantation of ICD's in patients with a prior MI and an ejection fraction of less than 30% has been shown to reduce mortality from 20% to 14% [3].
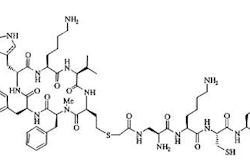
Cardiac resynchronization therapy has been shown to improve left ventricular (LV) function and reduce hospitalization and death in patients with advanced/chronic CHF and LBBB [1]. The current selection criteria for CRT are an LVEF < 35% and a widened QRS complex (>120 ms) [4,5]. CRT can improve clinical manifestations and quality of life, reduce hospitalizations for CHF, reduce complications, and risk of death (increase survival) [4,5]. Unfortunately, between 20-50% of patients do not respond to CRT [1,5]. Lower MIBG uptake (H/M ratio below 1.36) is associated with a higher likelihood for lack of response to CRT [4]. The lower MIBG uptake may reflect hearts with more severe myocardial damage that are less likely to respond to CRT [4]. Following successful CRT intervention, there is improved cardiac uptake of MIBG [4].
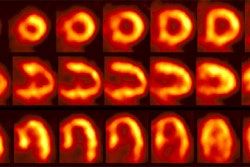
A widened QRS complex is indicative of electrical dyssynchrony, however, the presence of left ventricular mechanical dyssynchrony suggests patients that are more likely to respond to CRT [5]. Phase image analysis from gated cardiac SPECT examinations can be used to evaluate for the presence of LV dyssynchrony [5]. One added benefit is that additional prognostic information can also be obtained from the perfusion images [6]. Dyssynchrony can also be evaluated using tri-plane tissue Doppler imaging (TDI) to measure segmental myocardial velocities [6]. LV dyssynchrony of more than 65 milliseconds on tri-plane tissue Doppler imaging can also predict CRT response [6]. TDI is highly operator dependent, and 20% of patients have a suboptimal acoustic window [7].
Extensive LV scarring - or scar in the region in which the LV pacing lead is positioned (typically the posterolateral region)- can also result in a decrease likelihood for response to CRT (extensive scarring is predictive of lack of CRT response with a sensitivity of 83% and a specificity of 74%) [5]. This suggests that improvement in LV function is prohibited in the presence of extensive scar tissue [5].
Surgical revascularization can result in improved patient survival in patients that are shown to have myocardial viability.
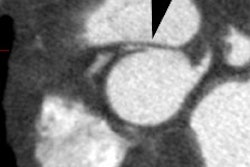
X-ray:
REFERENCES:
(1) J Nucl Med 2006; Thompson K, et al. Is septal glucose metabolism altered in patients with left bundle branch block and ischemic cardiomyopathy. 47: 1763-1768
(2) J Nucl Med 2007; Schinkel AFL, et al. Assessment of myocardial viability in patients with heart failure. 48: 1135-1146
(3) Radiology 2007; Wu JC, et al. Cardiovascular molecular imaging. 244: 337-355
(4) J Nucl Cardiol 2007; D'Orio Nishioka SA, et al. Cardiac sympathetic activity pre and post resynchronization therapy evaluated by 123I-MIBG myocardial scinitgraphy. 14: 852-859
(5) J Nucl Med 2007; Henneman MM, et al. Nuclear imaging in cardiac resynchronization therapy. 48: 2001-2010
(6) J Nucl Cardiol 2008; Chen J, et al Assessment of left ventricular mechanical dyssynchrony by phase analysis of ECG-gated SPECT myocardial perfusion imaging. 15: 127-136
(7) J Nucl Med 2007; Henneman MM, et al. Can LV dyssynchrony as assessed with phase analysis on gated myocardial perfusion SPECT predict response to CRT? 48: 1104-1111