Radiology 1993 Apr;187(1):45-49. Acute chest syndrome in sickle cell disease: CT evidence of microvascular occlusion.
Bhalla M, Abboud MR, McLoud TC, Shepard JA, Munden MM, Jackson SM, Beaty JR, Laver JH
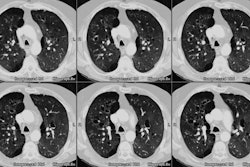
Patients with sickle cell disease often develop acute chest syndrome (ACS). Signs of ACS include chest pain, fever, prostration, and pulmonary opacities. Pneumonia and infarction have been implicated in the pathogenesis of this syndrome. Infarction as a result of microvascular occlusion and pneumonia are not easily differentiated with chest radiography or ventilation-perfusion scintigraphy. The authors evaluated the ability of thin section (3-mm) chest computed tomography (CT) to help diagnose microvascular occlusion in ACS and thus help differentiate two of its most likely causes. CT scans of the chest of 10 patients with moderate to severe ACS were retrospectively reviewed by two observers, who listed the number of bronchopulmonary segments showing consolidation; areas of ground-glass attenuation due to early hemorrhagic edema; and paucity or absence of small vessels, arterioles, and venules. In all patients, the degree of hypoxia was out of proportion to the extent of consolidation evident at chest radiography. The CT scans showed microvascular occlusion and areas of ground-glass attenuation in nine patients. Infection was ruled out in eight patients. High-resolution CT may play an important role in the initial evaluation and timely selection of an appropriate treatment regimen aimed at improving tissue perfusion, thus forestalling irreversible organ damage and chronic pulmonary arterial hypertension in patients with sickle cell disease.
PMID: 8451435, MUID: 93197528