Pulmonary Lymphangiectasia:
View cases of pulmonary lymphangiectasis
Clinical:
Pulmonary lymphangiectasia is a rare disorder that is seen more frequently in males. It occurs secondary to a developmental defect which results in obstructive, dilated lymphatics and subsequently "wet lungs" (ie: there is arrested lymphatic development). Patients may present with severe neonatal respiratory distress, cyanosis, and death. There are questionable associations with familial cases, Noonan's syndrome, and ichthyosis congenita [1].There are 3 forms of the disorder:
1- Isolated Pulmonary: The developmental defect is isolated to the pulmonary lymphatics. Felt to be related to failure of regression of the pulmonary lymphatics after the 16th week of gestation. It results in severe interstitial lung disease and has a poor prognosis. Rarely children may live beyond the neonatal period.
2- Secondary to Pulmonary Venous Obstruction: This form is associated with congenital heart disease and accounts for 30% of cases. Cardiac abnormalities include: Hypoplastic left heart, total anomalous pulmonary venous return type III, and pulmonic vein atresia.
3- Generalized: (Systemic)- Characterized by lymphangiectasia throughout the body. The pulmonary manifestations are typically mild. Patients may have an associated lymphangioma.
X-ray:
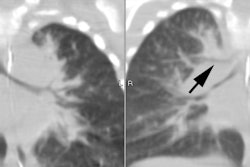
On CXR, pulmonary lymphangiectasia is characterized by hyperinflation and a diffuse, coarse, reticulo-nodular prominence to the lung markings. Focal cystic areas may be seen. Chylous pleural effusions may also be seen. If the disorder is systemic, UGI exam will demonstrate thickened small bowel folds due to enlarged submucosal lymphatics.REFERENCES:
(1) AJR 1999; Chung CJ, et al. Children with congenital pulmonary lymphangiectasia: After infancy. 173: 1583-1588