Chest radiography as a predictor of outcome in posttransplantation lymphoproliferative disorder in lung allograft recipients.
Pickhardt PJ, Siegel MJ, Anderson DC, Hayashi R, DeBaun MR
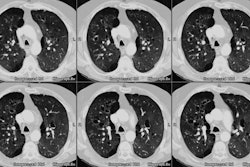
OBJECTIVE: The radiologic findings of posttransplantation lymphoproliferative disorder in lung transplant recipients have received little attention compared with the findings for recipients of other solid organ transplants. We describe the intrathoracic findings and explore whether the radiographic presentation can predict outcome. MATERIALS AND METHODS: Twenty-six patients (mean age, 32 years; range, 2-63 years; 18 female, eight male) with histologically proven lymphoproliferative disorder were identified from 518 lung transplantation patients, a 5.0% frequency. Chest radiographs, obtained within 1 week of diagnosis, were compared with baseline posttransplantation radiographs for all 26 patients and with chest CT scans for 20 patients. RESULTS: The interval between transplantation and diagnosis ranged from 6 weeks to 7 years (mean, 16 months; median, 6 months). The thorax was involved in 18 (69%) of 26 patients. A new chest radiographic abnormality was present in all 18 patients and provided the first indication of disease in 14 (78%) of 18 patients. The most common finding was a solitary pulmonary nodule, seen in nine (50%) of 18 patients. Other findings included multiple nodules, multifocal alveolar infiltrates, and hilar and mediastinal adenopathy. CT scans detected additional nodules and lymph nodes but did not show occult disease in any case that appeared normal on radiography. Eight (89%) of nine patients with solitary pulmonary nodules at presentation were alive 1 year after diagnosis, compared with six (35%) of 17 patients with other presentations (p < .01). CONCLUSION: Thoracic manifestations are present in most lung transplant recipients with lymphoproliferative disorder. Patients with solitary nodules have a better outcome in the first year after diagnosis than do patients with other presentations.