Sjogren's Syndrome:
View cases of Sjogren's syndrome
Clinical:
Sjogrens syndrome is a relatively uncommon chronic inflammatory autoimmune disease characterized by lymphocytic infiltration (T lymphocyte) of the exocrine glands [3,5]. The disease usually affects women (9:1) in the 4th or 5th decade of life [5]. Patients complain of xerostomia (dry mouth), keratoconjunctivitis sicca (dry eyes), and polyarthritis. It occurs most commonly in middle aged females (9:1).The disorder can be categorized as "primary" or "secondary". Secondary Sjogren's syndrome is commonly associated with other connective tissue disorders such as rheumatoid arthritis, systemic lupus erythematosis, and systemic sclerosis (scleroderma). Up to 95% of affected patients are rheumatoid factor positive and 80% have a positive anti-nuclear antibody test. Anti-La antibodies (anti-nucleoprotein antibodies) occur in about 40% of patients and are relatively specific for the primary form of the disorder. The ESR is elevated in 60% of cases. The zerostomia is the result of atrophy of the salivary and parotid glands. Biopsy of the affected glands typically demonstrates a lymphocytic infiltrate.
Various forms of lung disease may be identified in these patients
including
interstitial lung disease, small airway disease and
lymphoreticular
disease.
Interstitial lung disease occurs in 4 to 52% of patients and is
more
common
in secondary Sjogren's syndrome or in patients with primary
disease
with
extraglandular features such as Raynaud's, renal disease, or
intermittent
purpura [2]. Narrowing of both large and small airways by a
lymphocytic
mucosal infiltration has been documented and may account for
obstructive
ventilatory changes noted at pulmonary function testing [2].
Airway abnormalities (follicular bronchitis) are a common
manifestation of primary Sjogren syndrome with a frequency of
48-68% [6].
Lymphoreticular lesions associated with Sjogren's include lymphocytic interstitial pneumonitis (LIP), pseudolymphoma (now called mucosa associated lymphoid tissue lymphoma or MALTOMA), lymphoma, and amyloidosis.
MALTOMA occurs in about 25% of patients and represents a extraglandular polyclonal proliferation of plasma cells and lymphocytes. Histolgoically, there is preservation of the lymphoid architecture, which is helpful in distinguishing the lesion from lymphoma. The most common sites for MALT lymphoma are the salivary glands and occular adenexa [4]. About 5% of patients with Sjogren's (both primary and secondary disease) develop a lymphoreticular malignancy- most commonly a B-cell non-Hodgkins lymphoma [2,5]. The lymphoma primarily arises from the salivary glands [5]. Of the patients that develop lymphoma, pulmonary involvement can be found in 20% of cases, but isolated lung involvement is uncommon (4% of cases). Radiographically, pulmonary lymphoma associated with Sjogrens syndrome may appear as a diffuse interstitial process or as multiple nodular infiltrates [3].
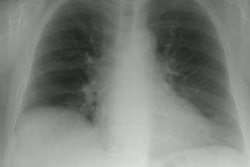
X-ray:
Computed tomography: CT is more sensitive than plain film in the detection of parenchymal abnormalities in patients with Sjogrens syndrome [3]. Abnormal findings can be identified by CT in 34% of patients with primary Sjogrens. When present, abnormal findings include fine reticular changes affecting the primarily the lower lobes, parenchymal lines, areas of ground glass attenuation, honeycombing, and bronchiolar abnormalities (bronchiolectasis and bronchial or bronchiolar wall thickening). Interstitial lung disease may be identified in up to 50% of patients, but it is more prominent in patients with secondary Sjogren's and it may be related to the associated connective tissue disease.REFERENCES:
(2) J Thorac Imag 1992; 7(2): 62-77
(4) AJR 2002; Tonami H, et al. Mucosa-associated lymphoid tissue
lymphoma in
Sjogren's syndrome: initial and follow-up imaging features. 179:
485-489
(5) Radiographics 2012; Capobianco J, et al. Thoracic
manifestations
of collagen vascular diseases. 32: 33-50
(6) Radiographics 2013; Egashira R, et al. CT findings of
thoracic manifestations of primary Sjogren syndrome:
radiologic-pathologic correlation. 33: 1933-1949