Pulmonary infections after bone marrow transplantation: clinical and radiographic findings.
Leung AN, Gosselin MV, Napper CH, Braun SG, Hu WW, Wong RM, Gasman J
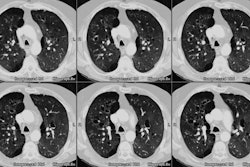
PURPOSE: To assess the clinical and radiographic findings of pulmonary infections diagnosed by using invasive means. MATERIALS AND METHODS: Fifty-nine episodes of pulmonary infection were diagnosed in 52 (7.2%) of a consecutive series of 725 adult bone marrow transplant recipients. Causative organisms, time of diagnoses, radiographic patterns, and mortality rates were reviewed. RESULTS: Cytomegalovirus and Aspergillus species were the two most common pathogens, accounting for 22 and 17 episodes, respectively. During the first 30 days after bone marrow transplantation, fungi caused the majority (nine [82%] of 11 episodes) of pulmonary infections; from days 31 to 100, viruses predominated (21 [62%] of 34 episodes). Recipients of allogeneic transplants had a higher probability of developing Cytomegalovirus pneumonitis than did the recipients of autologous and syngeneic transplants (P < .001). Radiographic findings of Cytomegalovirus pneumonia consisted of parenchymal opacification (90%) and innumerable nodules smaller than 5 mm (29%); in two patients, radiographs were normal. Nodules, masses, or nodules and masses, present in nine (69%) of the 13 patients with Aspergillus infection, were the most common radiographic findings in invasive aspergillosis. Bone marrow transplant recipients with a documented pulmonary infection were found to have a lower event-free survival than recipients without infection (P < .001). CONCLUSION: Opportunistic pathogens account for the majority of pulmonary infections requiring invasive diagnosis and tend to manifest at predictable times in the course of events following recovery from bone marrow transplantation. Cytomegalovirus, the most common pathogen, causes a spectrum of radiographic findings that includes normal findings. Occurrence of a pulmonary infection is associated with an increased mortality rate.