Radiol Clin North Am 1997 Mar;35(2):457-85
Colorectal cancer. Radiologic staging.
Thoeni RF.
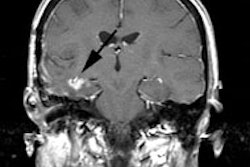
The role of conventional CT scan and conventional MR imaging in assessing
patients with colorectal tumors is now well established. Because both techniques
have an unacceptably low accuracy for identifying the early stages of primary
colorectal cancers (T1, T2N0 or N1 and early T3N0 or N1, or Dukes stage A, B1
and 2, and C1), their routine use for preoperative staging is not recommended.
This low staging accuracy is related to the fact that neither method can assess
the depth of tumor infiltration within the bowel wall and both have difficulty
in diagnosing malignant adenopathy. These distinctions are necessary in order to
determine correctly patient prognosis and tumor resectability. If the various
publications on CT scan and MR imaging staging of primary colon tumors are
summarized, a mean overall accuracy of approximately 70% can be established. The
sensitivity for lymph node detection of malignant lymphadenopathy is only about
45%. The sensitivity for detection of positive lymph nodes is better for rectal
tumors because any adenopathy in the perirectal area can be considered malignant
because benign adenopathy is not seen in this area. For the early stages of
colon cancer or recurrent tumor at the anastomotic site, endoscopic ultrasound
or TRUS is the method of choice. Both TRUS and MR imaging with endorectal coils
can demonstrate the various layers of the rectal wall, but the ultrasonographic
examination can be performed at lower cost and is less time-consuming. Despite
these limitations CT scan and MR imaging are useful for assessing patients
suspected of having extensive disease, including invasion of fat or neighboring
organs or metastatic spread to distant sites including, liver, adrenals, lung,
and so forth. CT scan and MR imaging are also helpful in the following ways: in
determining whether a patient will benefit from preoperative radiation or
whether a patient with rectal cancer can undergo a sphincter-saving procedure;
for designing radiation ports; and for detecting complications related to the
neoplasm, such as perforation with abscess formation or preobstructive ischemia
in patients with complete obstruction by tumor. In these cases, management often
is based on CT scan and MR imaging findings and cross-sectional follow-up
studies can establish the success of treatment. CT scan and MR imaging have a
premier role in the detection of recurrent colorectal cancer. CT scan and MR
imaging are superior to colonoscopy for diagnosing extrinsic mass-like tumor
recurrences and they are the only methods by which patients with total AP
resection can be fully evaluated. The overall accuracy of CT scan and MR imaging
for detecting recurrent colorectal tumors ranges from 90% to 95%. Following AP
resection, CT scan cannot reliably determine whether a soft tissue density in
the surgical bed represents recurrent tumor, and it is important to obtain CT
scan baseline studies 4 months after surgery and to repeat this examination at
6-month intervals. Scar tissue, even if initially masslike, shrinks over time
and after 1 year should be smaller and its margins more sharply defined. Any
apparent increase in size of a mass or any demonstration of adenopathy must be
considered an indication for biopsy. Recurrent tumors that do not extend to the
pelvis or abdominal sidewalls or invade bone or nerves can be resected. Subtle
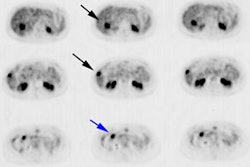
tumor recurrence or tumor foci in small nodes can be detected by PET scan and
immunoscintigraphy, but their future role in the diagnostic imaging of
colorectal cancer patients depends on the results of ongoing studies. Helical CT
scan has the advantages of fast volume scanning associated with optimal bolus
delivery, absence of artifacts related to motion, absence of missed slices, and
availability of reformations in multiple planes and three-dimensional
reconstruction (virtual reality). The role of this technique in patients with
colorectal neoplasms has not been defined. (ABSTRACT TRUNCATED)