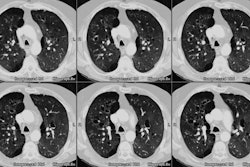
Pneumopericardium:
View cases of pneumopericardium
Clinical:
Pneumopericardium is typically seen in the setting of recent cardiac
surgery. Other
causes include closed (unusual) or penetrating chest trauma, barotrauma
seocndary to mechanical ventilation, and extension of infection or
tumor. Pneumopericardium is also seen in neonates undergoing mechanical
ventilation for
respiratory distress syndrome.
Tension pneumopericardium can occur in neonates, but the
condition is rare in adults. A tension pneumopericardium requires
emergent treatment with needle pericardiocentesis and possibly
placement of a pericardial drain [1]. Clinical signs of tension
penumopericardium include pulsus
paradoxus, tachycardia, and an increased central venous pressure with
decreased cardiac
output. Auscultatory findings include a characteristic "mill wheel"
murmur and muffled heart sounds [1]. Elevated ST segments and
low-voltage waveforms may be seen at ECG [1].
X-ray:
Pneumopericardium is usually manifested as a single band of gas that
may outline both
the left ventricle and right atrium- it is another cause of the
continuous diaphragm sign
also seen in pneumomediastinum. The band of radiolucency is sharply
marginated by the
pericardial sac and does not extend into the upper mediastinum or neck.
The fibrous
pericardium invests a portion of the ascending aorta, the superior vena
cava to the level
of the azygous arch, and the main and right pulmonary arteries and air
associated with
pneumopericardium may extend to these levels, but not beyond. Another
finding which helps
to distinguish pneumopericarium from pneumomediastinum is that the
location of pericardial
air will vary with patient position, while mediastinal air does not
shift. A "small heart sign" denotes tension pneumopericardium when
there is a sudden decrease in the size of the cardiac silhouette [1].
REFERENCES:
(1) Radiographics 2011; Katabathina VS, et al. Nonvascular,
nontraumatic mediastinal emergencies in adults: a comprehensive review
of imaging findings. 31: 1141-1160