Schwannoma (Neurilemmoma):
View cases of schwannoma
Clinical:
Schwannoma is the most common neurogenic tumor of the posterior mediastinum. The lesion arises from the nerve root sheath, extrinsically compresses the nerve fibers, and extends along the intercostal nerve [3]. Lesions that arise from the vagus, phrenic, or internal mammary nerves are located in the more anterior aspects of the mediastinum. It is generally a benign, slow growing tumor of a peripheral nerve which is usually encapsulated. Most patients are asymptomatic, but they may have radicular pain. Treatment is surgical and resection is curative. Malignant schwannomas are rare (2% of cases, although slightly more common in patients with NF1) and are characterized by rapid growth and local invasion, distant metastases are uncommon. Patients with malignant lesions are more likely to present with chest pain.
X-ray:
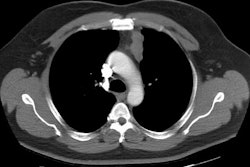
On CT the lesion appears as a low density, sharply marginated,
soft tissue, posterior
mediastinal mass typically in the para-spinous portion. There may
be intra-spinal extension
producing a "dumbbell" lesion in about 10% of cases. The lesion is
usually
round, or elongated in a horizontal direction following the
intercostal nerve. There may
be pressure erosion of the adjacent bony structures. Small foci of
calcification have been
reported in up to 10% of cases and this may primarily be in a
peripheral pattern [3]. If large, the lesion may be inhomogeneous
or cystic due to
areas of hemorrhage and necrosis within the mass.
A "split fat" sign refers to fat attenuation around the soft
tissue mass caused by displaced, but intact surrounding fat that
covers the neuromuscular bundle, indicative of a noninfiltrating
underlying neurogenic mass [3].
On MRI, schwannomas have low to intermediate signal on T1 images, and intermediate to high signal on T2 images [3]. The solid components of the lesion will enhance with gadolinium administration [3].
REFERENCES:
(1) Chest 1997; Strollo DC,
et al. Primary
mediastinal tumors. Part II: Tumors of the middle and posterior
mediastinum. 112: 1344-57
(2) Radiographics 2003; Rha SE, et al. Neurogenic tumors in the
abdomen:
tumor types and imaging characteristics. 23: 29-43
(3) AJR 2016; Pavlus JD, et al. Imaging of thoracic neurogenic tumors. 207: 552-561