Systemic Sclerosis (Scleroderma):
View cases of scleroderma
Clinical:
Systemic sclerosis is an autoimmune disorder characterized by excessive sollagen production, autoimmune induced inflammation, and microvascular injury [7] which may be initiated by an environmental antigen. A genetic predisposition has been identified (HLA-DR5 and HLA-DR3). The peak incidence is seen in patients between 45-64 years of age [8]. Reports suggest that black Americans may experience more severe disease than white Americans [8].The two main forms of systemic sclerosis are diffuse cutaneous and limited cutaneous disease. Both forms are more common in women (3:1 to 8:1 [8]) and there is no significant difference in mortality between the two forms (overall mortality at 10 years is about 40%). A less common sub-type is scleroderma sine scleroderma which is characterized by interstitial pulmonary fibrosis, but no skin manifestations.
Diffuse cutaneous disease: Patients with diffuse cutaneous disease demonstrate Raynaud's phenomenon, swelling of the hands and feet, hidebound skin changes usually affecting the trunk, and constitutional symptoms. Patients with diffuse disease have a significantly increased frequency of interstitial lung disease, as well as renal and cardiac involvement. Patients with diffuse cutaneous disease have a worse prognosis [4]. Anti-topoisomerase-1 antibodies (anti-Sci-70) are found in 30% of patients with diffuse disease and is associated with pulmonary fibrosis and an increased risk for malignancy. Only about 1% of patients develop pulmonary arterial hypertension.
Limited disease: Limited disease is slightly more common than the diffuse form (accounts for about 60% of scleroderma patients) particularly affecting older females. Skin involvement is limited to the hands, feet, face, and forearms. The characteristic CREST syndrome (calcinosis, Raynaud's, esophageal involvement, and telangiectasia), although seen in both diffuse and limited disease, occurs in most commonly in association with limited cutaneous systemic sclerosis. Anti-centromere antibodies (ACA) are identified in 82% of patients with limited disease. Pulmonary arterial hypertension is more common (up to 10% of patients) and tends to be more severe in patients with limited disease. PAH is also more commonly found in patients with Raynauds and changes compatible with PAH can be found in up to 50% of patients with CREST syndrome at autopsy [8].
Pulmonary involvement can be found in over 90% of patients with
systemic
sclerosis on HRCT. Pulmonary disease is more common in SS than in any
other
connective tissue disease. Interestingly, very few affected patients
are
symptomatic. Manifestations include interstitial pulmonary fibrosis,
pulmonary
vasculitis, pulmonary arterial hypertension (10-16% of patients [8]),
respiratory muscle weakness, pleural effusion, and
secondary
neoplasms. The frequency of lung cancer in patients with systemic
sclerosis
(both limited and diffuse forms) may be as high as 21% [1]. Patients
with scleroderma also have an increased frequency of breast cancer [8].
The most frequently encountered pattern of interstitial pneumonia is NSIP, but UIP also occurs frequently [8]. UIP associated with progressive systemic sclerosis is less aggressive and has a better prognosis than the idiopathic variety of the disorder. A one-year course of cyclophosphamide has been associated with improvement in pulmonary function and symptoms in patients with scleroderma related interstitial lung disease [6]. Treatment has also been associated with improvement in abnormalities on HRCT imaging [6]. Cyclophosphamide treatment, however, can be associated with an increased risk for bladder, hematologic, and skin cancers [6].
Approximately 10% of cases of scleroderma occur in children [3] and evidence of pulmonary abnormalities can be found in up to 90% of patients on HRCT, even when plain films appear normal [3].
Scleroderma involves the esophagus in 50%-90% of patients [4].
Esophageal
involvement can occur prior to skin changes. In this disorder there is
degeneration and atrophy of the smooth muscle in the esophagus (distal
2/3's) which is replaced by fibrosis. The neural elements, including
ganglion
cells, are normal. The muscular degeneration results in severely
decreased
LES tone which has two effects: It permits food to easily enter stomach
when the patients is erect, but allows also free reflux resulting in
peptic
esophagitis and eventually stricture formation. Patients may be
asymptomatic
or may complain of heartburn due to reflux. Dysphagia due to stricture
formation is a later manifestation. Due to the reflux, these patients
are
at an increased risk for Barrett's esophagus.
Small bowel findings include hypomotility from smooth muscle atrophy
and fibrosis, which leads to stasis, dilatation, and pseudo-obstruction
[9]. The "hide-bound" sign of
valvular packing is a fairly specific finding and may be seen in as
many as 60% of patients with scelroderma [9].
X-ray:
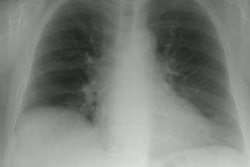
HRCT findings are very similar to those of UIP or NSIP. Systemic sclerosis can be suspected when interstitial lung disease is discovered in association with esophageal dilatation (found in 40-80% of cases). Mediastinal adenopathy is frequently associated with interstitial lung disease in patients with underlying systemic sclerosis. Adenopathy is seen in about 40% of patients with limited disease, and about 60% of patients with diffuse disease. Between 8% to 17% of patients with systemic sclerosis and mediastinal adenopathy will not have associated interstitial lung disease [2]. Traction bronchiectasis (due to fibrosis) and bronchiectasis secondary to chronic aspiration may also be identified.In children, HRCT findings include areas of ground glass attenuation, honeycombing, linear opacities, and sub-pleural micronodules (possibly due to follicular hyperplasia) [3]. Although mediastinal adenopathy in not uncommonly found in adults with systemic sclerosis, this finding has not been identified in children [3].
REFERENCES:
(2) J Thorac Imag 1992; 7(2): 30-45
(3) AJR 1998; Seely JM, et al. Systemic sclerosis: Using high-resolution CT to detect lung disease in children. 170: 691-697
(4) Radiology 1999; Pickhardt PJ. The "hide-bound" bowel sign. 213: 837-938
(5) Radiology 2004; Desai SR, et al. CT features of lung disease in patients with systemic sclerosis: comparison with idiopathic pulmonary fibrosis and nonspecific interstitial pneumonia. 232: 560-567
(6) Chest 2009; Goldin J, et al. Treatment of
scleroderma-interstitial lung disease with cyclophophamide is
associated with less progressive fibrosis on serial thoracic
high-resolution CT scan than placebo. 136: 1333-1340
(7) Radiographics 2011; Kanne JP, et al. Beyond skin deep: thoracic
manifestations of systemic disorders affecting the skin. 31: 1651-1668
(8) Radiographics 2012; Capobianco J, et al. Thoracic manifestations
of collagen vascular diseases. 32: 33-50
(9) Radiographics 2013; Bhavsar AS, et al. Abdominal manifestations of neurologic disorders. 33: 135-153