Lymphoproliferative disorders after lung transplantation: imaging features.
Rappaport DC, Chamberlain DW, Shepherd FA, Hutcheon MA
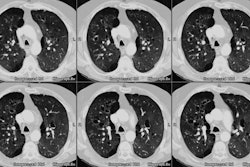
PURPOSE: To define the imaging features of lymphoproliferative disorders that occur after lung transplantation. MATERIALS AND METHODS: In a retrospective review of the cases of 246 patients who had undergone lung transplantation (62 single- and 184 double-lung transplants) between 1987 and 1997, the authors found nine patients (seven men and two women, aged 16-59 years [mean, 42.2 years]) with posttransplantation lymphoproliferative disorders. All imaging, clinical, and pathologic findings pertaining to these disorders were reviewed. RESULTS: Eight of the nine patients had isolated intrathoracic disease. The most common abnormality (six patients) was the presence of multiple, well-defined pulmonary nodules. These nodules, when multiple, had basilar and peripheral predominance. Other abnormal features included hilar or mediastinal adenopathy (two patients), a consolidated upper lobe (one patient), a pleural mass (one patient), and bulky abdominal lymphadenopathy (one patient with pathologically proved Hodgkin lymphoma). Three patients had nodules with a surrounding area of ground-glass opacity (halo sign), and one patient had multiple ill-defined areas of centrilobular opacity. Air bronchograms were not often seen, and pleural effusions were absent. CONCLUSION: The presence of well-defined pulmonary nodules in a patient who has undergone lung transplantation should raise concern about the possibility of posttransplantation lymphoproliferative disorder. In such cases, performance of pathologic studies should be expedited.