Swyer-James (MacLeod's) Syndrome:
View cases of Swyer-James syndrome
Clinical:
Swyer-James is a variant of post-infectious bronchiolitis
obliterans that is most commonly the sequela of a viral (adenovirus or RVS) infection during
infancy or early childhood. Mycoplasma infection has
also been implicated [5]. Swyer-James may also be
seen following measles, pertussis, tuberculosis, and mycoplasma infections [4].
There
is a necrotizing bronchiolitis (bronchiolitis
obliterans) which damages the terminal and
respiratory bronchioles and prevents the normal development of their alveolar
buds. Additionally, fibrosis (the result of the healing process) results in
bronchiolar obstruction that in turn leads to air trapping [1The syndrome is
characterized by unilateral hyperlucency with
associated decrease in the size and number of pulmonary vessels on the involved
side. Patients may be asymptomatic, or complain of recurrent URI's, wheezing or
cough, or dyspnea on exertion. Although classically
involving an entire lung, the disorder can be lobar or subsegmental.
Differential considerations for a unilateral hyperlucent lung include: Endobronchial foreign body, pneumothorax, congenital lobar emphysema, pulmonary artery hypoplasia/occlusion (no air trapping evident on expiratory images [3]), compensatory hyperinflation, or chest wall defect (Polland's syndrome).
X-ray:
On
CXR there is unilateral hyperlucency with a small
pulmonary artery and decreased vascularity on the
affected side. There is a prune tree appearance to peripheral bronchi. The
affected lung most commonly appears small, although hyperexpansion
due to collateral ventilation and air trapping may be seen [5].
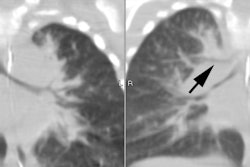
On
CT there are hyperlucent regions without surrounding walls (cysts and bulla
have walls) and the central pulmonary artery is small with decreased branching
and sparse vessels within the hyperlucent region. Expiratory scans demonstrate
air trapping in the involved areas. Bronchiectasis is
not necessarily a component of the disorder, although it is frequently seen in
the affected lung [2]. The presence of saccular bronchiectasis has been reported to be associated with an
increased risk for recurrent infection [4]. On ventilation scintigraphy
with xenon there is air trapping with delayed wash-in and washout from the
involved areas. Matching perfusion defects are identified.
REFERENCES:
(1) J Thorac Imag 1995, 10: p.236-54
(2) J Thorac Imag 1995; 10: p.255-67
(3) J Comput Assist Tomo 1997; 21 (4): 616-618
(4) J Comput Assist Tomo 1998; Lucaya J, et al. Spectrum of manifestations of Swyer-James-MacLeod syndrome. 22(4): 592-597
(5) Radiographics 2011; Dillman JR, et al. Expanding upon the unilateral hyperlucent hemithorax in children. 31: 723-741