Pulmonary complications after bone marrow transplantation: high-resolution CT and pathologic findings.
Worthy SA, Flint JD, Muller NL
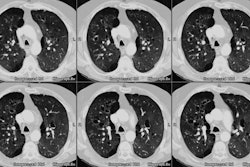
A wide variety of pulmonary complications occur in bone marrow transplant (BMT) recipients and are a major cause of morbidity and death. High-resolution computed tomography (CT) is excellent in the detection of pulmonary abnormalities, but these findings are generally nonspecific. However, the different complications, which reflect the immunologic status of the patients, occur in three phases. This pattern can be used to interpret CT scans. The neutropenic phase (up to 3 weeks after BMT) is characterized by fungal infections, notably angioinvasive aspergillosis, alveolar hemorrhage, pulmonary edema, and drug reactions. At CT, angioinvasive aspergillosis appears as a nodule surrounded by a halo of ground-glass attenuation; alveolar hemorrhage and drug reactions, as bilateral areas of ground-glass attenuation or consolidation; and pulmonary edema, as prominent pulmonary vessels, interlobar septal thickening, ground-glass attenuation, and pleural effusions. The second phase (3 weeks to 100 days after BMT) is dominated by cytomegalovirus pneumonia, which appears as multiple small nodules with associated areas of consolidation or ground-glass attenuation, and Pneumocystis carinii pneumonia, which appears predominantly as ground-glass attenuation. The late phase (more than 100 days after BMT) is characterized by bronchiolitis obliterans, bronchiolitis obliterans with organizing pneumonia (BOOP), and chronic graft-versus-host disease. In bronchiolitis obliterans, CT reveals bronchial dilatation and a mosaic pattern of attenuation; in BOOP, CT findings usually consist of patchy consolidation or ground-glass attenuation. If CT findings are considered in relation to the time elapsed after BMT, diagnostic options can be narrowed sufficiently to enable accurate diagnosis.
Publication Types:
Review
Review, tutorial