Hepatobiliary Imaging
Physiology
Hepatic cells secrete about 1 liter of bile per day. Bilirubin is the final degradation product of porphyrin metabolism, and its principal source is the catabolism of hemoglobin. Bilirubin is extracted from the plasma by the hepatocyte, conjugated with glucuronic acid, and excreted into the bile canuliculi. Conjugated hyperbilirubinemia usually indicates the presence of biliary obstruction. Common bile duct flow is solely passive, but the cystic duct may function as a variable resistor that actively regulates flow into and out of the gallbladder.
Radiopharmaceuticals
Tc 99m IDA (Iminodiacetic acid) analogs:
Tc-iminodiacetic acid derivatives are organic anions. These agents predominantly bind to albumin in the circulation and are carried to the liver. Protein binding helps to decrease renal excretion. Dissociation of the tracer from albumin takes place at the perisinusoidal space of Disse and the tracer enters the anion exchange pathway of bilirubin. Since the compounds share the same hepatic uptake and excretion pathways, IDA compounds are subject to competitive inhibition by bilirubin. IDA compounds are taken up by hepatocytes and are NOT conjugated prior to their excretion (they are excreted unchanged). In general, increasing the length of the alkyl chain substitution on the benzene ring of IDA, will increase the biliary excretion of the agent and decrease the renal clearence. This is because substitutions of non-polar groups on the phenyl ring make the molecule more lipophilic and the more lipophilic a compound, the greater its protein binding. (Protein binding prevents renal excretion and promotes hepatic uptake)
HIDA: dimethyl
- 85% excreted by the liver, 15% by the kidneys
- Good visualization at bili levels of 5-7 mg/dl
- Approximately 88% hepatic excretion, 10% renal
- Good visualization at bilirubin levels approaching 20
- An analog of lidocaine [3]
- m-3-bromo-trimethyl-IDA, has greatest resistance to displacement by bilirubin. Over 80% of the administered activity is cleared from the blood by liver hepatocytes within 10 minutes [5]. There is about 98% hepatic excretion of the agent [3]. The agent is excreted by the hepatocytes without metabolism or modification [5]. The agent is excreted into the bile by adenosine tri-phosphate dependent export pumps- the multidrug resistance associated proteins 1 and 2- without undergoing biotransformation during transit through the hepatocyte [4]. Excretion of the agent is not affected by elevated levels of serum bilirubin [5].
- T1/2 of uptake is about 6 minutes, and the T1/2 of excretion is about 14 minutes.
DISIDA: diisopropyl (Disofenin)
Disofenin: (Mebrofenin)
Technique
The patient should be fasting for 4 to12 hrs; prolonged fasting
may actually result in a false positive test (ie: failure to
visualize GB) due to bile shunting away from the full
gallblladder. Narcotics that act on the sphincter of Oddi should
be stopped 6 to 12 hours prior to the examination.For patients
that have not eaten in over 24 hours, Sincalide (0.02 ug/kg) can
be infused over one hour similar to that for a GBEF exam [6]. The
tracer should then be administered at least 30 minutes following
completion of the infusion to provide sufficient time for
gallbladder relaxation [6].
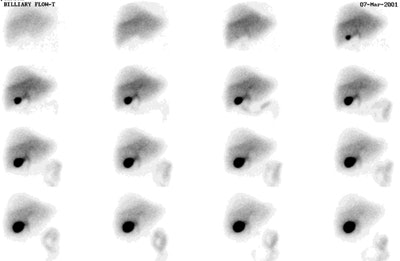
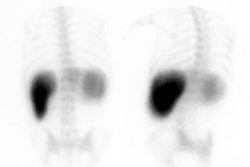
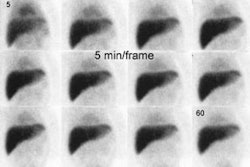
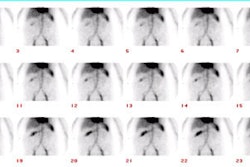
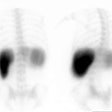
On the normal scan by about 5 minutes the liver activity should exceed cardiac blood pool, and by 10 minutes the cardiac blood pool activity should be gone. Persistent blood pool activity indicates hepatocellular dysfunction. Biliary activity is typically seen by 15 minutes and over 90% of normal studies demonstrate the gallbladder within 30 minutes. About 80% of normal subjects show small bowel activity within 60 minutes,and all show it within 90 minutes. If activity is seen within the gallbladder, but not in the small bowel by 90 minutes of the study, Sincalide may be used to expedite small bowel visualization and measure gallbladder ejection fraction. In patients with significant jaundice, do not confuse renal excretion for GB activity- always check lateral view as the GB will be anterior and renal activity posterior.
|
Normal Hepatobiliary Exam: A normal hepatobiliary exam demonstrating prompt hepatic tracer uptake and normal excretion into the gallballder and small bowel. There is breast attenuation over the upper portion of the right lobe of the liver. Click the image to view the cine exam (100KB). Case courtsey of Dr. Jamie Montilla, MD |
|
|
Gastric reflux of bile may be identified on the examination, and, if severe, this has been implicated as a cause of gastritis. Normal patients have less than 15% of actvity refluxed into the stomach. A large portion of this percentage is likely related to scatter and overlying loops of small bowel. Following a Billroth II reconstruction, it is not abnormal to see gastric reflux of bile. Quantitative analysis in these patients can show up to 25% enterogastric reflux normally. Reflux of more than 65% of activity is excessive, commonly associated with symptoms, and generally an indication that symptoms will be relieved following surgical diversion.
Cholecystokinin in hepatobiliary imaging
Cholecystokinin (CCK) is released endogenously by the duodenal mucosa in response to a fatty meal [2] (in response to fat, amino acids, and small polypeptides in the small intestine). The serum CCK rises and peaks during 20 to 30 minutes and remains elevated until there is no longer a stimulus for secretion [2]. The serum CCK level then returns rapidly to baseline due to it's rapid metabolism (serum half-life of 2.5 minutes) [2]. Gallbladder contraction is initiated when the serum CCK concentration reaches a threshold (which is considerably lower than the peak CCK level) [2]. CCK also acts to relax the sphincter of Oddi allowing bile to empty into the small bowel [2].
Sincalide (synthetic CCK) reproduces the active portion of CCK (the C-terminal octapeptide fragment). The most commonly administered dose is 0.02 ug/kg given by slow I.V. infusion (typically over 4 to 5 minutes, but 30 to 60 minute infusions have also been described for GBEF determination). Gallbladder contraction begins rapidly following sincalide infusion, with a maximal effect within 15 minutes. Since the serum half-life of Sincalide is only 2.5 minutes, the agent can be administered more than once during an exam.
Indications for the use of Sincalide include patient fasting for more than 20 to 24 hours (in order to empty the gallbladder of non-radiolabelled bile prior to the start of the exam) and the determination of GBEF (see below).
Actions of CCK include:
- Gallbladder contraction and relaxation of the sphincter of Oddi. Gallbladder contraction is threshold dependent and maximum contraction is seen 40 to 60 minutes after a meal.
- Stimulates secretion of bile and pancreatic enzymes.
- Increases jejunal, ileal, and, to a lesser degree, colonic motility.
- Increases pyloric tone thereby inhibiting gastric emptying.
- Decreases gastroesophageal sphincter tone.
Sincalide may alter biliary dynamics in patients with chronic cholecystitis so that the gallbladder appears sooner than 1 hour after injection. Prolonged biliary to bowel transit can be seen following the administration of sincalide due to preferential shunting of bile into the recently emptied gallbladder.
Morphine Augmented Cholescintigraphy:
Morphine can be used to decrease the time required to confirm acute cholecystitis. Dose: 0.04 mg/kg (Max. 2-3mg) given over a 3 minute infusion. Morphine may be administered after 45 minutes to 1 hour if the gallbladder is not visualized, and there is- 1) No evidence of CBD obstruction, and 2) Sufficient activity remains within the liver to allow for subsequent imaging, otherwise reinjection may be necessary.
Subanalgesic doses of IV morphine contract the sphincter of Oddi
and increase intrabiliary pressure [6]. Morphine can produce up to
a 10 fold increase in the resting pressure of the common bile duct
through contraction of the sphincter of Oddi. The subsequent rise
in common duct pressure results in preferential flow through the
cystic duct, if it is patent [6].Enterogastric reflux is not
uncommon, probably because of relaxation of the pyloric sphincter
[6]. Levorphanol or meperidine (demerol) could be theoretically
used if morphone is unavailable, but there are few published
reports to confirm its accuracy [6].
If GB has not filled by 30 after MSO4 injection the exam is felt to be diagnostic of acute cholecystitis. Visualization of the gallbladder 5 to 30 minutes after morphine is indicative of chronic cholecystitis. Overall, the sensitivity (96 to 100%) and specificity (81 to 100%) are very similar to the basic examination with delayed images.
There have been case reports of morphine producing a false-negative study (ie: visualization of the gallbladder despite the presence of acute cholecystitis), particularly in the setting of acute acalculous cholecystitis. False positive exams occur with a higher frequency in patients with severe intercurrent illness or long term parenteral nutrition [1] (Sensivitiy 94%, Specificity 70%). The lack of food entering the duodenum in these patients results in the absence of CCK mediated gallbladder contraction and bile stasis occurs in a distended gallbladder. Water resorption continues, eventually resulting in a gallbladder filled with thick, viscous sludge. The lower predictive value of the exam in this setting is likely related to a combination of factors including the inability of tracer to enter the sludge-filled gallbladder (despite CCK admistration), poor sphincter response to morphine in patients already on narcotics, and underlying intrahepatic cholestasis [1]. A false positive exam may also occur if there is insufficient tracer remaining In the liver and a booster dose may be necessary in some cases.
REFERENCES:
(1) Radiology 1990; Fig LM, et al. Morphine-augmented hepatobiliary scintigraphy in the severely ill: Caution is in order. 175: 467-473
(2) Radiology 2001; Ziessman HA, et al. Normal values for sincalide cholescintigraphy: Comparison of two methods. 221: 404-410
(3) J Nucl Med 2002; Krishnamurthy GT, Krishnamurthy S. Hepatic bile entry into and transit pattern within the gallbladder lumen: a new quantitative cholescintigraphic technique for measurement of its concentration function. 43: 901-908
(4) J Nucl Med 2007; Dinant S, et al. Risk assessment of posthepatectomy liver failure using hepatobiliary scintigraphy and CT volumetry. 48: 685-692
(5) J Nucl Med 2009; Adenosine triphosphate-binding cassette
subfamily C member 2 is the major transporter of the hepatobiliary
imaging agent 99mTc-mebrofenin. 50: 1140-1146
(6) J Nucl Med 2014; Ziessman HA. Hepatobiliary bscinigraphy in
2014. 55: 967-975