One of the most common elective medical procedures in the U.S. today is laser eye surgery, or laser-assisted in situ keratomileusis (LASIK). It’s advertised as a quick, practically risk-free operation that corrects nearsightedness, farsightedness, and astigmatism.
According to a June 28, 2001 report from USA Today, more than a million people are expected to opt for the procedure this year. But data from the Food and Drug Administration suggest that up to 5% of patients -- 50,000 -- may experience quality-of-vision complications, including fluctuating vision, decreased night vision, "aquarium" vision, corneal abrasions, muscle spasms, visual field defects, and dry eyes. Unsuccessful LASIK surgery can have devastating effect on a patient’s life; how much more can it damage the livelihood of people like radiologists, who use their eyesight daily to make crucial judgment calls?
It’s a question that sparked debate recently on AuntMinnie.com’s Residents Digital Community discussion board. Posters discussed the pros and cons of LASIK surgery for people who spend hours each day making fine distinctions between shades of gray that can dramatically affect their patients’ lives.
"I am not sure I would have this done being a radiologist. The other problem is the long- term outcome, i.e. 20 years down the road, that no one knows about. Your eyes are your skill. Why risk it?" one poster commented.
On the other hand, another poster reported nothing but stellar results: "I am six months out from my surgery. It is really great! I don't think it has compromised any part of my practice, diagnostic or interventional."
Yet the majority of the posts expressed concern about the procedure. AuntMinnie.com takes a look at what’s behind LASIK surgery and whether the benefits outweigh the risks.
A look at LASIK
LASIK is a type of refractive surgery that was developed to address corneal imperfections such as myopia, hyperopia, and astigmatism. It reshapes the cornea with an excimer laser.
Developed in the 1980s, the procedure incorporates the technique of keratomileusis, or cutting of the cornea, with the use of excimer lasers, which have been used in industry since 1971 and in ophthalmic surgery since 1983, according to the American Society of Cataract and Refractive Surgery. Excimer lasers produce pulses of ultraviolet light, each of which removes 1/4000 mm of tissue from the surface of the cornea. The FDA made its first clearances of excimer lasers for LASIK surgery in 1999.
The kindest cut
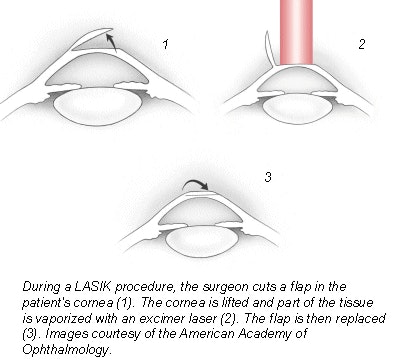
The surgery takes less than 30 minutes and is performed under local anesthesia. First, the eye is numbed and the lids held open with a speculum. A suction ring, with a cutting instrument called a microkeratome attached, is positioned over the eye, and high pressure is applied to create suction on the cornea.
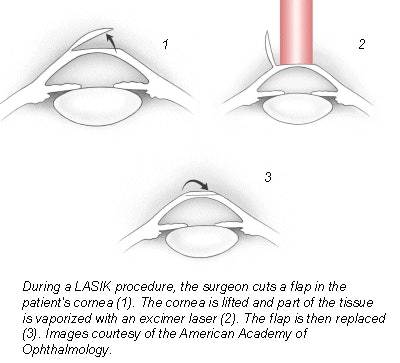
The surgeon uses the microkeratome to cut a flap in the cornea, leaving a hinge at the left end of the flap. The suction ring is then removed, and the doctor lifts the flap and folds it back on its hinge to allow the exposed tissue to dry. Although patients can see at this point in the procedure, they often experience varying degrees of blurred vision during the rest of the surgery.
The surgeon positions the laser over the patient’s stroma, the mid-section of the cornea, while the patient focuses on an additional light so as to keep the eye fixed on one spot. Using the laser, the doctor removes the amount of corneal tissue determined by measurements taken at the patient’s initial evaluation. When the tissue has been vaporized, the corneal flap is replaced, and a shield is placed over the patient’s eye to protect the flap because stitches are not necessary.
 |
Benefits and pitfalls
LASIK advocates insist that the many benefits of the procedure outweigh its risks. For those who are nearsighted, farsighted, or who have astigmatism, the surgery seems to offer an easy way to say goodbye to glasses forever. Since no corneal surface tissue is removed, post-operative pain tends to be minimal and there is less potential for scarring, which means that the correction is more stable. Most patients who undergo the procedure find that visual acuity is restored in a few days, and their eyes adjust within one to three months.
But concern about the procedure is valid, particularly for those with acute near- or farsightedness, according to Dr. Keith Kellum, an ophthalmologist in private practice in Houma, LA.
"Since there is a possible decrease in contrast sensitivity with LASIK, (the procedure) might pose a slightly increased risk for radiologists, whose livelihood depends on being able to differentiate between gray scales," Kellum said. "Someone with severe myopia could have more loss of contrast sensitivity, because when you have to correct more you have to ablate (the cornea) more."
Potential complications include loss of the corneal flap during or after the operation, the incision being too deep or shallow, infection of the cornea, and most frighteningly, loss of visual acuity from scarring or from the cut itself.
Fluctuations in vision can continue to occur up to three to six months after the surgery, according to the Council for Refractive Surgery Quality Assurance, which describes the procedure as a six-month process rather than a 20-minute operation. Those who experience these fluctuations beyond six months may have permanent complications that require more surgery.
Although the probability of serious, long-term complications are estimated at just 0.5% to 1.8%, the risks are still worth considering. And while the has become safer and more predictable over the years, the costs of that improvement have been borne by some LASIK patients, rather than by careful, peer-reviewed research and documentation, according to Surgical Eyes, a patient advocate organization. For radiologists and their patients, these costs may prove too much to bear.
By Kate Madden YeeAuntMinnie.com contributing writer
September 14, 2001
Copyright © 2001 AuntMinnie.com