Should low-dose CT replace chest radiography for determining whether patients scheduled for immunosuppressive therapy have latent tuberculosis? Not yet, according to German researchers, who believe chest radiography still has a role to play.
In a presentation at last month's ECR 2014, researchers from Klinikum Grosshadern at Ludwig Maximilian University in Munich discussed whether chest x-ray should be put out to pasture.
As radiology's oldest imaging modality, radiography has been supplanted by more powerful technologies such as CT for many clinical applications. Chest x-ray is still commonly used to screen patients with positive skin tests for tuberculosis (TB), but this application is being questioned by some due to the low yield of the studies.
For example, in a study presented at the RSNA 2013 meeting, researchers from New York questioned whether chest radiography should continue to be used for individuals with a positive purified protein derivative (PPD) skin test. They found that not a single incidence of active TB was indentified in a population of 904 cases.
In the ECR 2014 study, Ludwig Maximilian researchers approached the question from the importance of correctly diagnosing latent TB before patients start receiving immunosuppressive therapy. A false negative in such cases could lead to reactivation of TB due to the therapeutic drugs; on the other hand, using chemoprophylactics before therapy can lead to side effects and delays in patients with a false-positive diagnosis, according to Dr. Susan Notohamiprodjo.
Tools for detecting latent TB include chest x-ray and tests such as the Mantoux skin test and interferon-gamma release assays (IGRA). In doubtful cases, low-dose CT can be performed. But why not just use low-dose CT for all screening cases?
Notohamiprodjo and colleagues decided to perform a clinical study comparing chest radiography to low-dose CT in a group of adult patients seen at their facility from January 2010 through March 2013. Patients were included in the study if they received chest radiography and low-dose CT within one week of each other. Individuals were excluded if they had superposition of lung apices with huge infiltrations, atelectasis, or pleural effusion, or if they had lung fibrosis or cystic fibrosis.
In all, 81 patients were included in the study, 44 men and 37 women, with an average age of 55 years (range, 20-89 years). The indications for imaging included 28 cases of infection, as well as 27 patients with neoplasia, 11 with dyspnea, six with rheumatic disease, six for screening, and three for other reasons.
For chest radiography, the researchers used an imaging protocol of 125 kV and 500 mA, with a 1.15-mm focus film distance, and a moving grid; low-dose CT was conducted on a 64-slice CT scanner at 120 kV and 10 mA to 15 mA per slice, with a high pitch of 1.173.
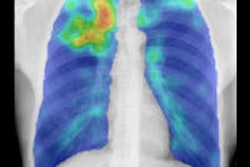
Images were reviewed by radiologists blinded to patient history and findings from the other modality. They looked for common radiological signs of tuberculosis infection: pleural thickening, fibrotic scars, and calcified lymph nodes, Notohamiprodjo said. Images were graded on the presence of two main factors -- pleural scarring/thickening and postspecific changes -- and they were also graded for diagnostic quality and image quality.
Compared with low-dose CT as the gold standard, chest radiography demonstrated high specificity, accuracy, and positive predictive value and moderate sensitivity, Notohamiprodjo said.
| Chest x-ray performance in tuberculosis screening | |||||
| Sensitivity | Specificity | Positive predictive value | Negative predictive value | Accuracy | |
| Pleural scars | 66.1% | 96.7% | 93.2% | 80.9% | 84.4% |
| Postspecific changes | 71.4% | 98.4% | 90.9% | 93.9% | 93.5% |
Radiography also had a false-negative rate of 13.4% for pleural scars and 5.2% for postspecific changes.
One big difference between chest radiography and CT was radiation dose, however: Chest x-ray produced an average radiation dose of 0.08 mSv (± 0.05), while low-dose CT produced a dose of 0.95 mSv (± 0.65).
Limitations of the study included the small number of patients, and its patient population had a high prevalence of pleural scars and postspecific changes. The clinical relevance of pleural scars is unclear as well, Notohamiprodjo noted.
Low-dose CT could evolve into a screening method in the future thanks to dose reduction technologies such as automated tube current modulation and model-based iterative reconstruction, she said. She concluded her talk by showing the ECR audience a chest CT image acquired using iterative reconstruction with a dose of 0.2 mSv.
"Our results justify chest x-ray being probably still a valuable screening method, and justify the use of low-dose CT in case of doubt, especially for patients with negative findings of pleural scars but with positive medical history, positive interferon-gamma release assays, or other postspecific changes," Notohamiprodjo said.