The number of postoperative radiographs performed after total shoulder arthroplasty could be cut drastically without affecting patient care, according to a new study published in the Journal of Shoulder and Elbow Surgery that questions the value of the imaging exam.
Researchers from the University of Virginia Health System found that performing a full schedule of postoperative x-rays cost a total of $248,281 in a population of 160 individuals -- nearly $1,800 per patient -- while doing little to change patient management.
"A lack of clinically meaningful impact from routine postoperative radiography does not justify per-patient expense, as routine imaging did not cause a change in postoperative management," wrote a team led by Dr. Ian Dempsey (J Shoulder Elbow Surg, January 25, 2017).
Improving outcomes
Shoulder arthroplasty has seen growing use in recent years as surgical techniques and patient outcomes have improved, the authors noted. Radiography has routinely been used to monitor patients in the first year after surgery, but falling complication rates have raised questions about whether this practice should be continued.
Indeed, previous research has hinted that routinely performing radiography after total shoulder arthroplasty doesn't add much to patient management. A study by Namdari et al in 2013 found that postoperative x-rays were both difficult to obtain and added little to medical utility, while similar studies also have found few clinical changes on x-ray after surgery in other anatomical areas, such as the hip and spine.
The researchers, therefore, chose to specifically focus on the usefulness of radiography in the first year after total shoulder arthroplasty. They examined 160 patients who received TSA surgeries from a single fellowship-trained surgeon at their institution between August 2010 and February 2015.
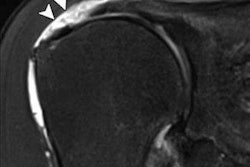
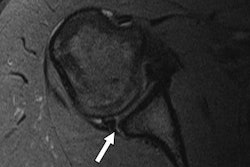
The institution's protocol was to perform a single postoperative Grashey anteroposterior-view x-ray of the shoulder in the postanesthesia care unit, with follow-up radiographs at two weeks, six weeks, four months, and one year after surgery. All images were interpreted by a musculoskeletal radiologist; clinical notes were reviewed to see if the images resulted in a change in patient management.
Dempsey and colleagues used the following radiologic parameters to determine if a change in patient management was warranted:
- Humeral or scapular fracture
- Hardware complication on the humeral or glenoid side, including early loosening or dissociation of components
- Any other radiographic feature that could include shoulder dislocation or displacement of lesser tuberosity osteotomy
The researchers determined the cost of the radiographs by obtaining data from the U.S. Centers for Medicare and Medicaid Services (CMS) for current procedural terminology (CPT) code 73030, two-view radiograph of the shoulder. Cost data included total cost, professional fee, and technical fees.
The rate of normal findings interpreted by the radiologist was as follows, delineated by the time at which the radiographs were acquired:
| Rate of normal x-ray findings for total shoulder arthroplasty | |
| Average follow-up period | Rate of normal findings |
| 1.8 weeks | 100% |
| 6.5 weeks | 96.8% |
| 14.9 weeks | 95.9% |
| 46.8 weeks | 95.2% |
In addition to the high rate of normal findings, no changes in patient management were made based on the routine radiographs, the authors reported.
"The data presented in this study found that routine radiography after primary TSA is not medically beneficial from a cost standpoint," they concluded. "Almost all radiographs in this study were normal, and repeated imaging failed to reveal any meaningful changes in postoperative care."
Cost-conscious care
In their discussion of the results, the authors noted that cost-conscious care and the appropriate allocation of resources are becoming "paramount for the long-term survival" of medical practices, especially as bundled payments become more common. At the same time, concerns about medical radiation also are prompting healthcare providers to limit patients' radiation exposure.
In noting the shortcomings of the study, the researchers noted the relatively small sample size and the fact that all the TSA procedures were performed by a single orthopedic surgeon. A larger study would be required to more definitively say that routine radiographs did not benefit patients.
Indeed, the institution has not eliminated routine radiographs entirely from their follow-up protocol; instead, they have limited the number of x-rays that are performed to two weeks, four months, and one year after surgery. And of course, radiographs should be acquired if any clinical concerns develop, such as a fall or trauma, the authors noted.