Elderly Seattle area patients who developed COVID-19 in February were made more vulnerable by comorbidities -- and 95% had abnormal imaging findings on admission to the hospital, according to a research letter published online March 19 in JAMA.
This added vulnerability to SARS-CoV-2, the virus that causes COVID-19, resulted in a high rate of mechanical ventilation (71%) and a mortality rate of 67%, wrote a team led by Dr. Matt Arentz of the University of Washington in Seattle.
"This study represents the first description of critically ill patients infected with SARS-CoV-2 in the U.S.," the team wrote. "These patients had a high rate of ARDS [acute respiratory distress syndrome] and a high risk of death, similar to published data from China. However, this case series adds insight into the presentation and early outcomes in this population and demonstrates poor short-term outcomes among patients requiring mechanical ventilation."
Until February, most of the COVID-19 cases reported were identified outside the U.S., but on February 19 one of the first U.S. deaths was reported at Evergreen Hospital in Kirkland, WA.
Arentz and colleagues outlined the clinical presentation, characteristics, and outcomes of 21 patients with COVID-19 admitted to the intensive care unit (ICU) of the hospital (patient mean age was 70). The cases were confirmed via nucleic acid testing with reverse transcription polymerase chain reaction (RT-PCR); patients were admitted between February 20 and March 5.
The study included anonymized patient data. The researchers reviewed laboratory results that were taken at ICU admission and at day five, as well as any chest x-rays; outcomes were assessed after five or more days of care in the ICU or at the time of the patient's death.
Most cases (86%) were in patients with comorbidities such as chronic kidney disease, congestive heart failure, and chronic obstructive pulmonary disease. Symptoms included shortness of breath (76%), fever (52%), and cough (48%); mean symptom onset was 3.5 days. Of the 21 patients, 17 (81%) were admitted to the ICU less than 24 hours after hospital admission.
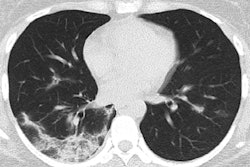
The researchers found that 95% of patients had abnormal chest x-rays on admission, with bilateral reticular nodular opacities and ground-glass opacities as the most common findings.
| Top 5 chest x-ray findings on hospital admission | |
| Findings | No. of patients (%) |
| Bilateral reticular nodular opacities | 11 (52.4%) |
| Ground-glass opacities | 10 (47.6%) |
| Pleural effusion | 6 (28.6%) |
| Peribronchial thickening | 5 (23.8%) |
| Focal consolidation | 4 (19%) |
At 72 hours postadmission, 86% of patients had bilateral reticular nodular opacities and 67% ground-glass opacities. In addition, 15 patients (71%) developed ARDS and were put on mechanical ventilation, and half of these patients developed severe ARDS by 72 hours.
As of March 17, the mortality rate among study patients was 67%; 24% of patients remain critically ill, and only 9.5% have been discharged from the ICU, the group wrote.
The study findings confirm that older people are at higher risk of death from COVID-19, the authors concluded.
"This study provides some initial experiences regarding the characteristics of COVID-19 in patients with critical illness in the U.S. and emphasizes the need to limit exposure of nursing home residents to SARS-CoV-2," they wrote.