A simple chest x-ray scoring system for assessing lung inflammation severity in COVID-19 patients helps doctors perform triage in underresourced countries, according to a study published July 30 in Advances in Clinical and Experimental Medicine.
Polish researchers used a five-point chest x-ray scoring system developed in 2015 to help clinicians of varying experience in settings with poor healthcare resources assess the severity of acute respiratory infections, and found it is also helpful for situations like the COVID-19 pandemic.
"In situations where a radiologist is unavailable to provide a quick evaluation, the interpretation of the severity of inflammatory abnormalities by a referring doctor serves as a valuable diagnostic and prognostic guideline," wrote a team led by Dr. Marta Rorat, PhD, of Wroclaw Medical University.
Chest x-ray for lung assessment has been considered a basic diagnostic tool at the triage stage during the COVID-19 pandemic, but its performance compared to CT -- which is significantly more sensitive -- has not been widely validated. Access to CT is restricted in many medical centers, particularly in field hospitals and in countries where health services are insufficient.
Rorat and colleagues investigated the usefulness of a simple chest x-ray scoring scale to assess the presence and severity of inflammation in the course of COVID-19. They also evaluated the possibility of nonradiologist physicians interpreting the presence and degree of inflammation in the lungs on their own. The study consisted of a retrospective analysis of chest x-ray records and images of 152 consecutive patients between 19 and 96 years old who were hospitalized with SARS-CoV-2 infection between March and April 2020.
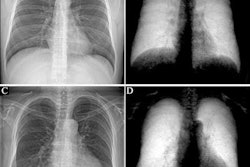
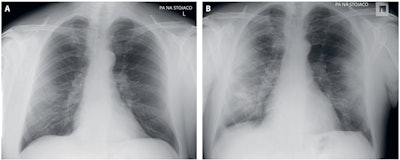 (A) April 10, a 53-year-old man, the fourth day after the onset of symptoms (cough, fever, oxygen saturation 97%); chest x-ray: unilateral, focal, peripheral patchy consolidation -- ground-glass opacity in the right lung; five-point scale score: 3. (B) April 17, chest x-ray: peripheral multifocal diffuse patchy consolidations in the right and left lung; five-point scale score: 4. Image and caption courtesy of Advances in Clinical and Experimental Medicine.
(A) April 10, a 53-year-old man, the fourth day after the onset of symptoms (cough, fever, oxygen saturation 97%); chest x-ray: unilateral, focal, peripheral patchy consolidation -- ground-glass opacity in the right lung; five-point scale score: 3. (B) April 17, chest x-ray: peripheral multifocal diffuse patchy consolidations in the right and left lung; five-point scale score: 4. Image and caption courtesy of Advances in Clinical and Experimental Medicine.To assess the severity of lung inflammation, the scoring system was used independently by a radiologist as well as an infectious disease specialist who underwent a short training session based on validated radiological images.
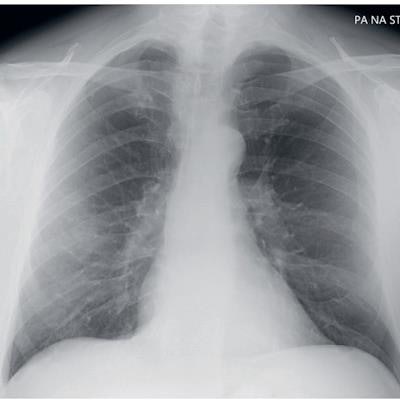
In 77 of 152 cases, the chest x-ray revealed inflammation features, with bilateral abnormalities found in the majority (62.3%) of cases. Lower lung lobes were involved more often than the upper ones, and the left lobe more often than the right one, the researchers found.
| Performance of a 5-point chest x-ray scale for assessing severity of inflammatory changes in the lungs by reader type | ||
| Chest x-ray score | Radiologist reader | Referring physician reader |
| 1 (Normal) | 75 (49.3%) | 73 (48%) |
| 2 (Patchy atelectasis) | 11 (7.2%) | 10 (6.6%) |
| 3 (Focal alveolar consolidation) | 21 (13/8%) | 20 (13.2%) |
| 4 (Multifocal consolidation) | 38 (25%) | 40 (26.3%) |
| 5 (Diffuse alveolar changes) | 7 (4.6%) | 9 (5.9%) |
In addition, the intensity of the abnormalities using the scale correlated with the persistence of symptoms: A positive and statistically significant correlation was found between the five-point scale and dyspnea, decreased oxygen saturation, elevated C-reactive protein, ferritin, D-dimer, lactate dehydrogenase, and alanine aminotransferase activity.
Currently, there are no standards for evaluating a chest x-ray in patients with COVID-19 and reports on the frequency of occurrence and the type of changes are still scarce, the authors noted. Given this study, they suggested in a setting such as the COVID-19 pandemic, radiologists could conduct training for referring clinicians as well as being helpful in cases of uncertain images.
"At the peak of a pandemic, when the system is overwhelmed, quantifying lung abnormalities accurately can be performed by a referring physician with a substantial agreement in respect to radiological evaluation," Rorat and colleagues concluded.