Significant inequities in placement and retrieval of inferior vena cava filters (IVCF) are evident for venous thromboembolism (VTE) patients in the U.S., according to research published April 27 in the Journal of the American College of Radiology.
After reviewing Medicare data for patients diagnosed with VTE from 2015 to 2018, a research team from Boston Scientific and the University of Pittsburgh found a number of disparities in IVCF placement and retrieval rates based on patient demographics, comorbidity burden, and geographic region.
"Given that patient demographics and geographic care location may affect IVCF retrieval, the findings provide insight into more intensified strategies before and after insertion to ensure compliance with professional medical society guideline recommendations for retrieval in at-risk populations," wrote the authors, led by first author Abimbola Williams from Boston Scientific and senior author Dr. Michael Jaff of the University of Pittsburgh Medical Center Presbyterian Hospital.
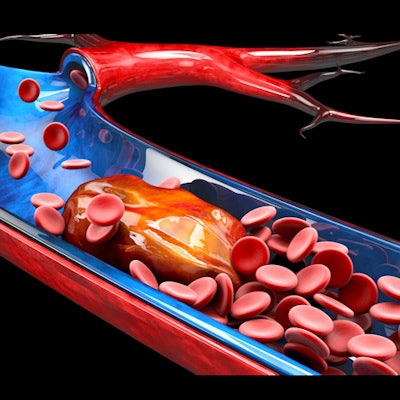
In patients newly diagnosed with VTE, inferior vena cava filters are often considered for patients who have contraindications or failures for anticoagulation treatment. To assess for population-based disparities in placement and retrieval of IVCFs, the researchers searched the Medicare 100% Standard Analytic Files for patients with index VTE diagnoses between 2015 and 2018.
Of the 516,978 patients with index VTE diagnoses, 5,864 (1.1%) received an IVCF. Retrieval procedures were performed in 1,884 (32.1%) of these patients.
The median time to receive an IVCF placement was 24 days from the index VTE diagnosis. Of those who underwent retrievals, these procedures were performed a median of 103 days after placement.
After performing Cox regression analysis, the researchers found several characteristics associated with higher rates of IVCF placement procedures:
- Index VTE diagnosis at outpatient facility: hazard ratio = 2.11 versus diagnosis at inpatient facility
- Index VTE diagnosis at "other" facility: hazard ratio = 1.56 versus diagnosis at inpatient facility
- Higher baseline Elixhauser comorbidity score: hazard ratio = 1.07 per 1-unit increase
- Age ≥ 75 years: hazard ratio = 1.26 versus ages 65-74
- Care received in the South: hazard ratio = 1.21 versus care received in the Midwest
Several variables were associated with lower rates of an IVCF retrieval procedure:
- Care received in the South: hazard ratio = 0.65 versus Midwest
- Care received in the Northeast: hazard ratio = 0.71 versus Midwest
- Index VTE diagnosis at outpatient facility: hazard ratio = 0.77 versus inpatient setting
- Male gender: hazard ratio = 0.83
- Higher baseline Elixhauser comorbidity score: hazard ratio = 0.95 per 1-unit increase
In other findings, Black patients experienced a longer wait (114 days), on average, than white patients (100 days) for a retrieval procedure, but this difference was not statistically significant (p = 0.115). The researchers also didn't discover any significant associations with either facility- or county-based characteristics and IVCF placements or retrievals.
"Although we did not find significant differences by race and facility [accountable care organization] status, variations in IVCF placement and retrieval by the site of VTE service were observed, suggesting that facility practices and characteristics may play a role in the use of IVCFs," the authors wrote.
As they don't require retrieval, bioconvertible IVCFs could contribute to eliminating disparities in retrieval rates, according to the authors.
"Future research on minimizing disparities in IVCF placement is warranted," they concluded.