Radiologic technologists performing portable chest x-ray imaging are in dire need of support, says a group in New York. The call to action follows a study that found quality failures may be present in nearly half of images acquired at their hospital, most during night shifts.
Stony Brook University clinicians analyzed a set of portable chest x-ray images acquired over a two-week period at their hospital and found that 46.2% were too poor in quality for accurate interpretation by a radiologist.
"This represents a staggering error rate. Just this number alone further emphasizes the need for intervention to improve [portable chest x-ray] imaging," wrote corresponding author Dr. Michael Jin, a radiology resident, and colleagues (September 15, Cureus).
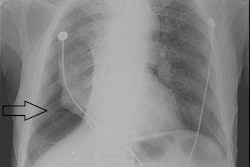
Portable chest x-rays have become widely used in hospitals across the U.S., not only for patients who are too sick to be transferred to the radiology department but also for routine floor patients. Patient rotation, foreign body overlying anatomy, and anatomy out of the field of view can have detrimental impacts on the quality of these exams.
Although preventable, these "quality failures" are common and may lead to interpretative and diagnostic errors for radiologists, the authors wrote. Moreover, with imaging volumes increasing, it is only becoming more difficult for technologists to consistently capture high-quality films for radiologists to interpret, the group wrote.
In this study, the researchers first quantified the baseline error rate in these exams at their hospital and determined the potential causes of the errors, and then proposed various hospital-wide interventions to better support radiology technologists.
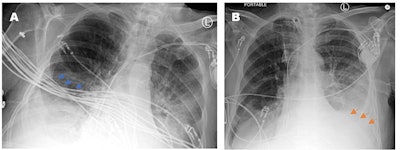 Two portable chest x-rays from a patient acquired at different times of the same day. The rotated and mispositioned film (A) cuts off the left cardiophrenic angle, which ended up concealing a large left-sided pleural effusion (orange arrows). The cardiac silhouette appears exaggerated and the EKG wires (blue arrows) severely obscure evaluation of the right lower chest and the right lower lobe airspace opacities. Image courtesy of Cureus.
Two portable chest x-rays from a patient acquired at different times of the same day. The rotated and mispositioned film (A) cuts off the left cardiophrenic angle, which ended up concealing a large left-sided pleural effusion (orange arrows). The cardiac silhouette appears exaggerated and the EKG wires (blue arrows) severely obscure evaluation of the right lower chest and the right lower lobe airspace opacities. Image courtesy of Cureus.The group culled 500 portable chest x-rays of adult patients admitted between July 12, 2021, and July 25, 2021. The x-rays were evaluated by radiology residents for failures in technical image quality and categorized into various metrics, including the degree of rotation and obstruction of anatomical structures.
Out of the 500 images evaluated, 231 were problematic (46.2%). Of these, 28% were from the day shift, 24% from the evening shift, and 48% were from the night shift, according to the findings.
"This shows that more support needs to be allocated to the night shift as it has a significantly higher error rate than the other shifts," the authors wrote.
In addition, 43.5% of the problematic films with a repeat portable chest x-ray within one week showed there were technical problems impacting the ability to detect pathology. Key issues that led to poor image quality included improper patient positioning, foreign objects covering anatomy, and variances in technologists' training, the authors wrote.
After collecting this data, the researchers organized a focus group involving six technologist managers to illuminate key barriers to quality imaging.
One key issue was that some technologists did not have the physical strength to move sick and overweight patients in ICU beds, resulting in poor image quality, the authors found. Also, when certain machines, medical devices, and wires interfered with their ability to capture images, technologists were often unsure about how each of the medical devices could be moved appropriately.
Third, given that patients have unique body habitus, varying states of health, and different past medical and surgical histories, the authors confirmed that technologists each take a slightly different approach when performing the exams, depending on the patient. They noted that these slight variations in approach to position and technique can also ultimately compromise image quality.
Moving forward, the authors have proposed three interventions to provide support to technologists to improve the diagnostic quality of the imaging, as follows:
- A longitudinal educational curriculum involving didactic sessions
- Adding nursing support to assist technologists
- Adding an extra layer of verification by internal medicine residents before sending the films to the radiologist
Solutions such as simply adding more floor staff and reducing imaging requests may work well in theory, but there are many drawbacks (costs, complexity) that make implementing them in a hospital setting difficult, the authors noted.
Future studies will evaluate the impact of the interventions they propose at Stony Brook University, they wrote.
"Additionally, educating technologists about commonly used medical devices in the ICU is important so they feel more comfortable moving them when capturing [portable chest x-rays]. Teaching technologists positioning strategies during special use cases such as specific immobilizations or heavier patients may also be of high value," Jin and colleagues concluded.