Radiology residents are up to the task of diagnosing emergency cases of pneumothorax on portable chest x-rays, compared with attending radiologists, according to a study by Pakistani researchers published September 27 in Cureus.
A group at Aga Khan University Hospital in Karachi analyzed the level of agreement between on-call radiology residents and attending radiologists when diagnosing pneumothorax on portable chest x-rays acquired in emergency settings. They found a high level of agreement between the groups.
"Pneumothorax is a medical emergency, so its timely and accurate diagnosis is essential for the management of this life-threatening condition," wrote corresponding author Dr. Junaid Iqbal, an assistant professor of radiology.
Pneumothorax is the presence of air or gas in the cavity between the lungs and the chest wall, which can cause the collapse of the lung. Chest x-ray is usually readily available and has high accuracy in detecting the condition. Rather than transporting patients from emergency settings to radiology departments, however, portable chest x-ray is commonly used to diagnose pneumothorax.
As part of their training in teaching and university hospitals, on-call radiology residents are responsible for the preliminary diagnosis of imaging, with attending radiologists then usually reviewing the cases the following morning. Although resident education is important, patient care cannot be compromised, the authors wrote.
Moreover, previous studies are mixed when it comes to comparing agreement between clinicians and radiologists when interpreting portable chest x-rays. In this study, the researchers aimed to identify the discrepancy rate between residents and attending radiologists at their hospital.
The group included 174 portable chest x-rays of patients acquired in the emergency room and intensive care units at their hospital that had been labeled positive for pneumothorax by a radiology resident and attending radiologist. Of the 174 patients, 139 (79.9%) were male and 35 (20.1%) were female. The mean age of patients was 45.6 years old.
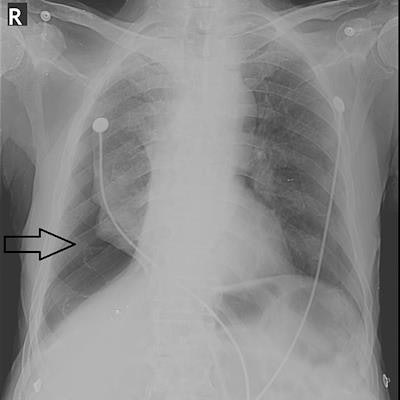
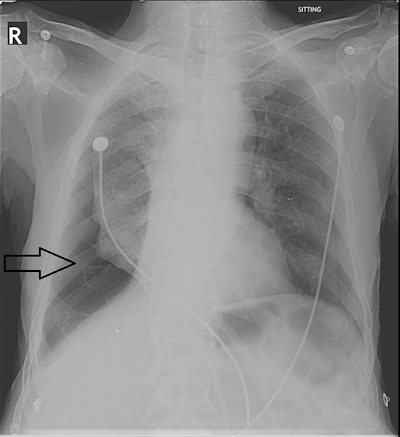 Right-sided pneumothorax (black arrow) reported by both the resident and the attending radiologist. Image courtesy of Cureus.
Right-sided pneumothorax (black arrow) reported by both the resident and the attending radiologist. Image courtesy of Cureus.According to the results, pneumothorax was reported by residents in 164 (94.25%) cases, while the attending radiologist reported it in 167 (96%) cases. The remaining 4% of cases were ultimately diagnosed on a chest CT scan. Concordance between the on-call residents and attending radiologists was 92.5% (p = 0.008), the researchers reported.
"The overall discrepancy rate between residents and attending radiologists in diagnosing pneumothorax is 7.5%, which is comparable with other published studies that have compared resident and attending radiologist interpretations," the authors wrote.
They noted an additional discovery over previous studies that the residency year of the postgraduate residents had a substantial impact on their accuracy in diagnosing pneumothorax on the portable chest x-rays. As the experience of the residents increased (from PGY-1 to PGY-4), the rate of correct diagnosis of pneumothorax also increased, and the discrepancy rate decreased, the authors found.
Ultimately, the experience of working during on-call hours and making independent decisions in challenging cases is essential to completing residents' training and education, and the goal of any residency program is to strike a balance between patient care and maintaining a good educational experience during an overnight call, the authors wrote.
In life-threatening and emergency cases, clinicians need to decide the management based on their own interpretation without having the opportunity to interact with radiologists.
"During on-call hours, radiology residents can safely identify and diagnose pneumothorax, so its management can be started without delay," Iqbal and colleagues concluded.