VIENNA - Differentiating liver lesions can be difficult in contrast-enhanced spiral CT, especially when lesions are very small and lack obvious markers for malignancy such as tendrils or feeder vessels. Different contrast-enhancement patterns could theoretically help differentiate among tumor types, but external factors such as cardiac function, blood viscosity, and patient size all work against differentiation -- to the point where natural attenuation differences can't be quantified.
As a result, different tumor types such as focal nodular carcinomas (FNC) and hepatocellular adenomas (HCC) might look different on CT, but not consistently and not for the right reasons.
At today's liver imaging sessions of the European Congress of Radiology, Dr. Andrea Ruppert-Kohlmayr discussed a new technique she developed with her colleagues at University Hospital of Graz, Austria. The technique uses standard-density values to exclude the influence of cardiac output and other factors on enhancement measurement of normal liver parenchyma and liver lesions, allowing different enhancement patterns to be quantified.
"The purpose of our study was to find a relatively simple way to measure contrast enhancement without the influence of external factors," Ruppert-Kohlmayr said. "Now the question is, do we need a quantitative measurement of enhancement? We don't need it when the lesion is acute [i.e., in cysts or solid perfused lesions] and enhancing quite a lot. But we need it if we want to use measurements of relative enhancement for differentiation of lesions."
The quantitative enhancement level that defines attenuation depends on the amount of contrast entering the organ and the lesion, respectively. The amount of contrast that reaches an organ or lesion is influenced by CT protocol parameters such as delay time, flow rate, the amount of injected contrast, and the localization of the venous line. It is also influenced by external factors, such as cardiac function, blood viscosity, and other patient factors like body weight and size, Ruppert-Kohlmayr said.
"We can partly exclude the influences of the CT protocol parameters when we equalize them for all patents. But the exclusion of external factors is not possible under natural conditions," she said. Thus, the team set out to find a formula that represented constant values for external factors, then use the resulting values to exclude those factors.
"Our idea was that if the aortic attenuation (were) equal in all patients, the same amount of contrast agent (would) enter the lesion if we have equal conditions and exclude all external factors," Ruppert-Kohlmayr said. "Therefore, we calculated the attenuation value in an organ or lesion that would be measured the next time when aortic attenuation would always have a certain always fixed equal attenuation value."
The researchers analyzed multiphasic helical CT scans in 27 patients with 45 histologically proven focal nodular hyperplasia (FNH) and 6 patients with 18 hepatocellular adenomas. The patients underwent unenhanced, arterial and portal-venous phase single-slice spiral CT on a Siemens Somatom Plus 4 scanner. Slice thickness was 8 mm, and pitch was 1.5 with reconstruction interval of 4 mm. Iodinated contrast (150 mm) was injected with a flow rate of 1 mm/s in the arterial and portal-venous phases. The field of view was the entire liver.
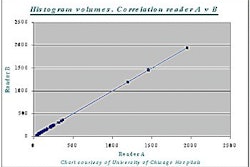
The group then measured attenuation of the lesions and liver in all patients in all three phases. In addition, density in the arterial and portal-venous (pv) phase was measured in the aorta at the level of the celiac trunk (TCa and TCpv). The cohort mean-value (mTC) was derived from all density values in all phases. The measured density of liver parenchyma and lesions was standardized by multiplying them with the following standardization factor: mTC/TA and mTC/TCpv for the portal-venous phase, Ruppert-Kohlmayr said.
"We measured aortic attenuation, the mean value in each contrast phase, and used this value as the reference attenuation," she said. "The ratio between this value and the measure of aortic attenuation in a certain patient gave the correcting factor of the attenuation. This factor was, for example, higher when the patient had a lower measure of aortic attenuation than the reference value, meaning less contrast agent had reached the level of celiac trunk."
The calculations resulted in an mTC value of 250 HU for the arterial phase and 130 HU for the portal-venous phase. The final step was to correct all measured TCa and TCpv values by the calculated values.
Ruppert-Kohlmayr and colleagues calculated the following standardized density values:
- Arterial mean value (mv): 80.29 HU (range: 48.21-123.1)
- Portal venous phase -mv: 105.43 HU (range: 73.41-146.8)
- Focal nodular hepatocarcinoma (1) mv: 117.91 HU (range: 86.3-147.6), (2) mv: 112.08 HU (61.4-123.75)
- Hepatocellualar adenoma (1) mv: 80.09 HU (range: 61.78-94.9), (2) mv:110.23 HU (range: 73.28-126.8)
"Attenuation in the arterial phase is much higher in focal nodular hyperplasia than in hepatocellular adenoma and in liver parenchyma, respectively," Ruppert-Kohlmayr said. Based on histologic results, the method was 98% accurate in determining tumor type based on attenuation differences in the arterial phase.
"To conclude, hepatocellular carcinomas and focal nodular hyperplasias can be differentiated by quantitative evaluation of relative enhancement," she said. "You have different enhancement characteristics in the arterial phase, and to get results without the influences of external factors on enhancement measurement we found a simple method that can be easily applied... not only on the liver, but probably on all other organs."
By Eric Barnes
AuntMinnie.com staff writer
March 4, 2001
Click here to post your comments about this story. Please include the headline of the article in your message.
Copyright © 2001 AuntMinnie.com