CHICAGO - Chest CT has proven to be the modality of choice in diagnosing inhalation anthrax. Radiologists from three facilities in the U.S. that have been on the front lines of the current war on bioterrorism offered their insights to attendees of an RSNA "hot topic" session Wednesday.
The session was moderated by Dr. Jeffrey Galvin, chief of chest and mediastinal imaging at the Armed Forces Institute of Pathology in Washington D.C. Galvin briefed the approximately 700 attendees on the history and pathology of anthrax (Bacillus anthracis), and outlined the progression of the disease once it finds a human host.
Dr. Daniel Seckinger of Miami’s Cedars Medical Center shared his experience in diagnosing inhalation anthrax. The patient, a 73-year-old Hispanic male who had delivered mail to the index-case patient of the current attacks, was admitted with cough, marked worsening of fatigue with lethargy, onset of exertional dyspnea, fever, sweats, and mild abdominal pain.
A chest x-ray taken on October 1 showed left upper and lower lobe infiltrates consistent with pneumonia and a small left pleural effusion. However, on October 2, a second chest x-ray revealed extensive left-lung infiltrates and pleural effusion. On October 5, CT of the chest showed bilateral effusions and multilobar pulmonary consolidation but no significant mediastinal lymphadenopathy. The patient tested positive for anthrax on a blood screen and ciprofloxacin was administered. Approximately three weeks later the patient was discharged from the facility.
Dr. James Earls presented the results of two cases handled by the Fairfax Radiology Centers in Fairfax, VA. On October 19, a 56-year-old man arrived at the emergency department of the Inova Fairfax Hospital in Fairfax, VA, complaining of flu-like symptoms (fever, chills, chest heaviness, and a minimally productive cough of three days’ duration).
He identified himself as a postal worker, and the emergency-room physicians ordered a posteroanterior (PA) projection chest x-ray and a chest CT study. The initial evaluation in the ER revealed a widened mediastinum on the chest radiograph, and an order to rule out anthrax was sent to the radiology department.
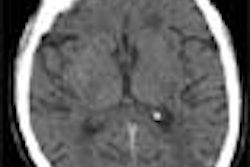
Dr. Donald Cerva Jr., the radiologist on duty, noted that the patient’s x-ray showed hilar and mediastinal masses. He also observed left-side hilar adenopathy and a small left infiltrate. A non-contrast, 7 mm slice thickness CT was ordered. Cerva observed a profuse and slightly hyper-attenuating paratracheal, anteroposterior (AP) window, subcarinal, hilar, and azygo-esophageal recess lymphadenopathy. In addition there was diffuse mediastinal edema, bilateral pleural effusions, bibasilar airspace disease more pronounced on the left, and thickened peribronchial tissue (seen best on lung windows).
The following morning, a second postal worker, also a 56-year-old man, who worked at the same distribution center as the first patient, was admitted to Inova with a three-day history of progressively worsening headache, muscle aches, and a slight cough. Because he was linked epidemiologically to the index case of inhalation anthrax at the institution, a chest radiograph and chest CT scan were ordered by the ER physician.
Dr. Elise Berman, the radiologist on duty, was aware of the earlier findings made by Cerva. She reviewed portable AP chest films and observed a widened mediastinum, bilateral hilar masses, bilateral pleural effusion, and perihilar airspace opacities.
A noncontrast CT scan was performed on the patient using the same chest protocol as the previous days’ patient. Berman noted the similar profuse and slightly hyper-attenuating paratracheal, AP window, subcarinal, hilar, and azygo-esophageal recess lymphadenopathy that Cerva had observed a few hours earlier in the first patient.
She also saw diffuse mediastinal edema, bilateral pleural effusions, and thickened peribronchial tissue. However, the patient’s images showed bibasilar airspace disease more pronounced on the right. The patients were started on a regimen of ciprofloxacin, rifampin, and clindamycin and were discharged from the facility within the next three weeks.
"Chest x-rays may be misinterpreted. We found CT to be absolutely critical in making the diagnosis of inhalation anthrax," Earls said of his group’s experience with the disease.
Dr. Christopher Krol of Lenox Hills Hospital in New York City agreed with his fellow radiologists about the possibility of misinterpreting chest x-rays. In the case admitted to his facility on October 25, a 61-year-old Asian woman who worked in the supply room of a New York City hospital, the chest x-ray was initially interpreted as showing pulmonary venous congestion with bilateral pleural effusions. The ER physician who interpreted the film initiated therapy for congestive heart failure.
Her therapy was changed to levofloxacin for atypical pneumonia as an echocardiogram showed normal ejection fractions and her respiratory status worsened. A CT scan of the chest, performed 16 hours after admission, showed mediastinal lymphadenopathy, massive mediastinal bleeding, thickened bronchial mucosa, and bilateral pleural effusions, said Krol.
The presenters shared with the audience the following diagnostic criteria for inhalation anthrax imaging:
Chest x-ray
- Widened mediastinum
- Bilateral hilar masses
- Bilateral pleural effusion
- Perihilar airspace opacities
Noncontrast routine spiral CT
- Profuse and slightly hyper-attenuating paratracheal, AP window; subcarinal, hilar, and azygo-esophageal recess lymphadenopathy
- Diffuse mediastinal edema
- Bilateral pleural effusions
- Bibasilar airspace disease more pronounced on left or right
- Thickened peribronchial tissue (seen best on lung windows)
By Jonathan S. Batchelor
AuntMinnie.com staff writer
November 29, 2001
For the rest of our coverage of the 2001 RSNA meeting, go to our RADCast@RSNA 2001.
Copyright © 2001 AuntMinnie.com