Virtual colonoscopy, it seems, is here to stay. Its accuracy has begun to approach that of traditional colonoscopy, yet with fewer risks and several advantages. And with the advent of multidetector CT scanners, better software, and more versatile workstations, VC's diagnostic value has increased steadily.
Even if the twin bugaboos of bowel prep and insufflation are still needed for now, the procedure is poised to become far easier for patients. Virtual colonoscopy has clealy reached some sort of critical mass. But there are still issues left to resolve, large trials awaiting results, and much work left to do.
In a presentation last week at the Digestive Disease Week meeting in San Francisco, Dr. Judy Yee from the University of California, San Francisco, offered a compelling view of VC's value in the detection of adenomatous polyps and colorectal cancers. In a wide-ranging talk, she discussed her own considerable experience with virtual colonoscopy, and that of her colleagues in the field.
Exposure
First introduced in 1994, virtual colonoscopy was made possible by the development of spiral CT, which enables data to be acquired volumetrically, Yee said. In recent years, the introduction of multidetector scanners has greatly improved VC's diagnostic abilities.
"With the MDCT scanner we're actually able to scan down to 1 mm, and we're able to pick up some of the smaller polyps and some of the flat lesions," Yee said. The optimal CT protocol requires thin collimation (5 mm or less), mAs less than 150 kVp, subsecond scanning, and a minimum 50% overlap when reconstructing images.
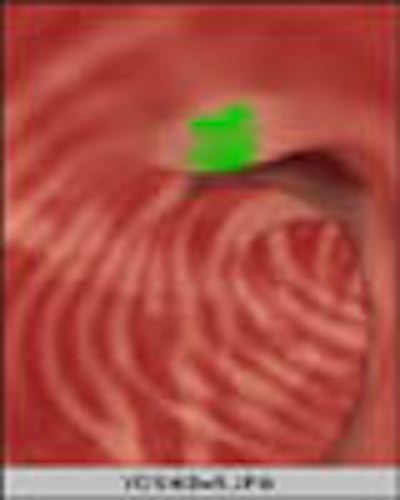
The CT scan must be performed in two positions, supine and prone. Images must be acquired in a single breathhold, which isn't a problem for multidetector scanners, she said. Axial, coronal, and sagittal images can be viewed in traditional and zoomed modes, and using multiplanar reconstructions. Different 3-D display modes include real-time endoluminal views. Viewing can be manual, semi-automated or automated.
"Most radiologists use the axial (2-D) view in magnifying format. However, a 3-D view is important for problem-solving," Yee said. "It's key that the software allow for easy switching between all four modes."
Patient prep
Patients must still undergo colonic cleansing and dietary restrictions prior to virtual colonoscopy, she said. The traditional prep agent is polyethylene glycol, but there are others, including magnesium citrate and sodium phosphate preparations, as well as bisacodyl stimulant laxative used in combination with other agents. A recent study by Macari et al compared residual fluid in two common agents.
"This study showed that there is more residual fluid on the colon exams with the use of polyethylene glycol versus phospho-soda," Yee said. "Therefore, saline products are actually preferred when performing virtual colonoscopy," although these are contraindicated in patients with heart and kidney disease (Radiology, January 2001, Vol. 218:1, pp. 274-277).
After prep comes bowel distension. Patients are placed on the CT table and a small tube is introduced into the rectum. The bowel is distended for imaging using room air or CO2.
"In initial studies using room air, they noticed that some patients were experiencing a significant amount of discomfort after getting off the CT table because of the colonic distension, and this introduced pain and discomfort," Yee said. "Therefore, some of us switched over to carbon dioxide."
Early studies also commonly used antispasmodic or antisperistaltic agents such as glucagon hydrochloride. However, the agents didn't really improve colonic distension or polyp detection, she said, so they're no longer recommended (AJR July 1999, Vol. 173:1, pp. 169-72; European Radiology March 2002, Vol.12:3, pp. 525-530).
Intravenous contrast
The use of intravenous contrast increases the cost and time required to perform virtual colonoscopy. VC is designed to be a fast, noninvasive screening exam, so radiologists don't use contrast routinely, Yee said. In a study by Morrin and colleagues, contrast significantly increased the exam's sensitivity for medium-sized polyps, but not of small and large-sized polyps (Radiology, December 2000, Vol. 217:3, pp. 765-767).
Prone and supine
VC patients must be scanned in both prone and supine positions. Dual positioning helps ensure adequate colonic distension, especially in the sigmoid colon, and enables the radiologist to distinguish polyps from mobile stool, she said. Chen et al compared single-position scans to prone and supine scans compared together. Imaging in both positions improved sensitivity both by patient and by polyp. When patients were scanned in one position, only 52% of the patients had adequate distension. When scans of both positions were considered together, 87% of patients had adequate distension (AJR, March 1999, Vol. 172:3, pp. 595-599).
Extracolonic findings
"Radiologists are required to look at the entire CT scan. That's basically a noncontrast CT of the abdomen and pelvis, so we do detect significant extracolonic findings," Yee said, citing a study by Hara and colleagues. "There's an 11% incidence of highly important colonic findings. Seventy percent of the patients went on to further imaging; 2.3% of the patients needed surgery because of the extracolonic findings," which included a renal mass, lung nodules, even a pneumothorax. The additional cost of workup was $7,324; the mean cost was just $28 per patient (Radiology, May 2000, Vol. 215:2, 353-357).
VC performance
Direct comparisons of the largest studies (Yee et al, Fenlon et al, Hara et al, Fletcher et al) are complicated by the use of different methodologies and protocols. Different reporting methods include patient matching, or more rigorous comparisons by polyp.
Cobbled together, these studies show overall sensitivities of 83%-100%, with specificity of 93%-100% by patient, and sensitivity of 75%-100% by polyp. By-polyp detection of medium-sized polyps (5-9 mm) averaged 80%-82%. Virtual colonoscopy also does an excellent job in detecting colorectal cancers: 8 of 8 in Yee's study (below), for example.
In Yee et al, direct polyp matching yielded sensitivity of 90% for polyps 10 mm and larger, 80.1% for polyps 5 to 9.9 mm, and 59.1% for polyps smaller than 5 mm (Radiology, June 2001, Vol. 219:3, pp. 685-692).
In Fenlon et al, virtual colonoscopy showed 91% specificity for polyps 10 mm and larger, 82% specificity for polyps 6-9 mm in size, and 55% specificity for polyps 5 mm and smaller (NEJM, November 1999, Vol. 11:341, pp. 1496-5030).
In Fletcher et al, the best results showed sensitivity of 85% for polyps 10 mm or larger, and 88% for polyps from 5 to 10 mm (Radiology, September 2000, Vol. 216:3, pp. 704-711).
In Hara et al, sensitivity was 89% for polyps 10 mm and larger, with similar results for polyps 5 mm and larger (Radiology, May 2001, Vol. 219:2, pp. 461-465).
Yee listed four multicenter trials in progress. Together they are expected to provide a clearer picture of VC's performance in large numbers of patients.
Pros and cons
"Virtual colonoscopy has proved valuable in cases of incomplete or failed colonoscopy," she said. "In the setting where the gastroenterologist cannot reach the cecum, the VC exam is able to demonstrate additional asynchronous carcinomas, as well as additional polyps."
Because it is noninvasive, VC is less risky than traditional colonoscopy. And it's fast -- as quick as a 10-second scan on her institution's 8-row multidetector scanner. It can be performed in patients with distal occluding lesions and in those with tight strictures. And in comparison to sigmoidoscopy, VC is a total colon exam.
On the other hand, VC results have been disappointing in the detection of smaller polyps and flat lesions, although the results are improving with the use of multidetector CT, Yee said. There is still considerable patient discomfort, which has led to the use of CO2 instead of room air. The procedure requires additional radiologist training, she said.
False-positive results can occur due to pseudolesions, retained stool, bulbous folds, diverticula, and other causes. False negatives can occur due to poor colonic distension, flat lesions, and poor image quality.
Radiation is an important concern, though in one study virtual colonoscopy at 70 mAs was found to yield about half the dose of a standard abdominal and pelvic scan, Yee said. (AJR, May 1997, Vol. 168:5, pp. 1181-1184).
"There are very few published studies evaluating patient tolerance or experience, and the results are frankly discrepant," Yee said. Results appear to vary depending on how the questionnaire is written, who administers it, how much sedation is given in traditional colonoscopy, whether oxygen or CO2 is administered in VC, and other factors.
Yee said she participated in a study wherein patients reported more pain and discomfort after virtual colonoscopy than after colonoscopy. "At the 24-hour mark there was actually a reversal of trend, with patients preferring virtual colonoscopy, although this was not statistically significant," she said. (Gastrointestinal Endoscopy, September 2001, Vol. 54:3, pp. 310-315).
Another study found the opposite: 82% of patients preferred virtual colonoscopy, and 69% found colonoscopy to be more painful and more difficult, she said (Radiology, February 2002, Vol. 222:2, pp. 337-345).
As for cost effectiveness, Sonnenberg and colleagues concluded that in order to compete with colonoscopy, VC needs a compliance rate that's 15%-20% better than colonoscopy's, at a cost no greater than 54% of the cost of traditional colonoscopy (American Journal of Gastroenterology, August 1999, Vol. 94:8, pp. 2268-2274).
"Given these results," Yee said, "I think that we as radiologists have to look at this and ask ourselves if this is potentially doable."
Looking ahead
A number of innovations are underway to improve the performance of virtual colonoscopy, including a prepless exam in which the patient ingests oral iodine or barium fecal tagging agents combined with electronic cleansing software that digitally subtracts fecal matter from the CT images, Yee said.
New display options, such as Mercator map projections, enable the radiologist to see more of the mucosal surface. Software is being developed to automatically segment the colon. The translucent viewing mode can help distinguish polyp from stool. Investigators are also working to develop displays that distinguish different types of polyps, such as adenomas from hyperplastic polyps. Computer-aided detection schemes will help automate the polyp-detection process, she said.
Yee concluded her talk by listing the five top issues facing virtual colonoscopy.
"We have to verify the performance in a screening (or) asymptomatic population," she said. "Radiologist standards have to be established, for both the performance of VC as well as the interpretation of VC. What is a good cutoff size for a significant polyp in virtual colonoscopy? (The answer) will directly impact the screening interval."
Patient acceptance needs to be reevaluated, particularly with the use of CO2 insufflation and prepless VC, she said. Researchers must determine an acceptable cost -- one that will make VC acceptable to large numbers of patients.
"So finally, virtual colonoscopy is here," she said. "It's really here to stay. It's the responsibility of the radiologist to perform the study well, to interpret the study well, but virtual colonoscopy is really a cooperative effort between radiologists and gastroenterologists, to ensure that there's an easy and effective referral system for patients who are found to have a lesion."
By Eric BarnesAuntMinnie.com staff writer
June 3, 2002
Copyright © 2002 AuntMinnie.com