With this article we continue our series of white papers on radiologic patient positioning techniques for x-ray examinations. The monthly series explores each of the major modalities. If you'd like to comment on an article or contribute an installment, please e-mail [email protected].
The contrast study of the large bowel, also called the lower gastrointestinal (LGI) series, is commonly performed using a barium enema. It is a valuable diagnostic tool that helps detect abnormalities in the large intestine. The barium enema, along with colonoscopy, remains standard in the diagnosis of colon cancer, ulcerative colitis, and other inflammatory diseases of the colon. There are two basic radiological methods of examining the large intestine by means of contrast enemas: a single-contrast method and a double-contrast method.
 |
Barium sulfate is the most common type of contrast media used for a barium enema. It is important to choose a barium suspension of appropriate density and viscosity for barium enema. If the viscosity of the barium suspension is too high, the examination will be prolonged, the filling of cecum and right colon will be difficult, and the drainage of barium will be inadequate. A standard mixture used for single-contrast barium enemas ranges between 15%-25% weight-to-volume (500 cc of barium sulfate is mixed into 1,500 cc tepid water to produce a 12%-20% solution).
A double-contrast barium enema uses a thicker barium with a weight-to-volume (w/v) concentration between 75%-95% or higher. Some patients require glucagon during the examination. Glucagon is a hypotonic drug used to achieve relaxation of colon. Colonic relaxation diminishes patient discomfort, accelerates the examination, and decreases incontinence.
Choice of contrast medium and indications for examination
The choice between the single- and double-contrast barium enema is the prerogative of the radiologist, and is an educated decision based on the condition of the individual patient and the clinical problem to be solved.
The single-contrast barium enema is preferable for the very young, the very old, the seriously ill, or the very disabled patient. Such patients are usually unable to stand on their own or to turn 360º when lying down. The method is often used for suspected obstruction, fistulization, and evaluation of the distal colon after colostomy.
 |
The double-contrast barium enema is preferable in patients with a family or personal history of colon neoplasia, in patients suspected or known to have inflammatory bowel disease, and in the search for the etiology of anemia, weight loss, or hematochezia.
The use of biphasic examinations (a double-contrast examination followed immediately after evacuation by low-density barium or a limited double-contrast evaluation of a difficult segment identified in single contrast) should be considered when a given examination is incomplete or equivocal.
 |
Water-soluble contrast medium should be used for patients with suspected perforation and for patients with suspected anastomotic leak.
Contraindications
Contraindications to the use of any barium enema include:
- Suspected perforation of the colon or pneumoperitoneum (an iodinated water-soluble contrast material should be used instead of barium).
- Generalized peritonitis.
- Gas in the bowel wall.
- Toxic megacolon.
- Biopsy of the colon after rigid sigmoidoscopy. A biopsy through the flexible fiber-optic endoscope for a superficial mucosal biopsy is not a contraindication. A barium enema can be performed on the same day as an endoscopy, providing a deep biopsy has not been made.
- Recent polypectomy by colonoscopy.
- Acute diverticulitis or other acute inflammatory bowel disease. In these patients, barium enemas should be delayed until medical management has had time to quiet the inflammation.
- A suspected abscess or fistula (an iodinated water-soluble contrast material should be used instead of barium).
 |
Patient preparation
- The day before the exam, the patient consumes a liquid nutritional supplement without fiber for breakfast, lunch, and dinner. This provides calories without residue.
- At 2 p.m. on the day before the exam, the patient drinks 12 oz (35.5 cl) of magnesium citrate, then drinks 8 oz (20 cl) of water every hour until 6 p.m., when four 5-mg bisacodyl laxative tablets are taken.
- The patient then drinks 8 oz (20 cl) water at 7 p.m., 8 p.m., and 9 p.m. on the day before the exam.
- A 10-mg bisacodyl suppository is unwrapped and inserted into the rectum between 6-7 a.m. on the morning of the exam.
 |
| Reprinted from Merrill’s Atlas of Radiographic Positions and Radiologic Procedures, 9th edition, Ballinger and Frank, page 149 (figure 17-116), copyright 1999 Mosby, with permission from Elsevier Science. |
Supplies
- Glucagon.
- 1-cc syringe (for glucagon).
- 18-gauge needle (for drawing glucagon), 25-gauge needle (for injecting glucagon).
- Tourniquet.
- Alcohol swab.
- Small bandage.
- Barium sulfate 500-600 cc (105% w/v for double-contrast barium enema).
- Barium sulfate 500-600 cc (85%-100% w/v for single-contrast barium enema).
- Barium enema bag with wide tubing (to allow flow of dense barium).
- Double-contrast enema tip with retention cuff.
- Cuff innator (for enema tip retention cuff).
- Lubrication jelly.
- Pneumatic bulb (to inflate colon) for double-contrast study.
A scout film is taken of the anteroposterior (AP) abdomen. If sufficient retained stool is visualized on the scout film, consider rescheduling the patient for the following day and repeating the bowel preparation or performing a cleansing enema. Residual stool can obscure small colonic lesions.
 |
Radiation
- Fluoroscopy: 750 mrad/min.
- Spot films: 70 mrad per spot film.
- kVp: single contrast -- 110 kVp, double contrast -- 90 kVp.
 |
Rectal tube insertion procedure
- Describe the tip insertion procedure to the patient.
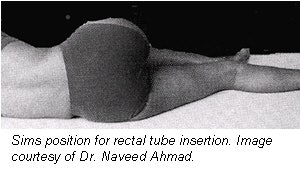
- The patient is asked to roll onto the left side and lean forward. The right leg is flexed at the knee and hip and is placed in front of the left leg. The left knee is comfortably flexed. This is called the Sims position. The goal is to relax the abdominal muscles and decrease pressure within the abdomen.
- Before insertion, the barium-sulfate solution should be well mixed. Allow barium to flow through the tubing and from tip to remove any air in the system.
- After wearing gloves, coat the enema tip well with water-soluble lubricant.
- Advise the patient to relax and take deep breaths. On expiration, insert the rectal tube gently into the anal orifice and direct the tube anteriorly 1-1 ½ inches (2.5-3.8 cm). The total insertion should not exceed 1 ½ inches (3 to 4 cm). Do not force the enema tip.
- After the rectal tube is inserted, tape it in place to prevent slipping. Do not inflate the retention balloon unless directed by the radiologist.
- Ensure that enema bag is no more than 24 inches (60 cm) above the table.
- Ensure tubing stopcock is in the closed position and no barium flows into the patient.
- Notify the radiologist as soon as everything is ready for the examination.
- Radiologist inflates the rectal balloon if necessary, observing with fluoroscopy to ensure placement proximal to the internal sphincter.
 |
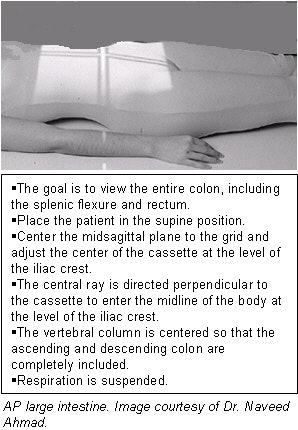
Patient positioning, imaging techniques for routine single-contrast barium enema
The basic principle for performing an accurate single-contrast barium enema is radiography of the colon so that all segments of the colon are clearly seen without overlapping loops. It is also necessary that each segment of colon be seen at fluoroscopy and on at least two films so that any suspected lesion can be verified.
This is accomplished by a combination of fluoroscopy and compression spot films of the entire colon, as well as bucky films of the entire colon. Compression spot filming is employed to thin out the barium column so that a small lesion, such as a polyp, can be easily seen. However, the rectum and the pelvic loops of the sigmoid colon are not amenable to compression. A through examination incorporates the following procedures and film sequences.
 |
Spot films
- Rectum. Use a 10 x 12-inch (25 x 30-cm) image receptor (IR). After insertion of the rectal tube with the patient in Sims position tilt the table head up (20º-30º), release the control clip until the enema flow fully distends the rectum, then image the rectum in both the AP and left lateral projections. Continued filling risks barium flooding the entire colon and terminal ilium, and can obscure the rectosigmoid colon.
- Sigmoid colon. Use a 10 x 12-inch (25 x 30-cm) IR. After imaging the rectum, run more barium and image the sigmoid in the left posterior oblique (LPO) and right posterior oblique (RPO) projections.
- Flexures. Use a 10 x 12-inch (25 x 30-cm) IR. With the table in the horizontal position, release the control clip and run more barium to opacify both flexures, oblique the patient to open, and image splenic flexure in RPO projection and hepatic flexure in LPO projection.
- Cecum. Use a 10 x 12-inch (25 x 30-cm) IR. Keeping the patient in the AP position, deliver more barium until the cecum is filled, and image with and without compression in AP projection. The ileocecal valve must be seen to ensure complete filling of the colon.
- Entire colon. Palpate the entire colon with a lead glove to look for masses under fluoroscopy and obtain spot films if needed.
 |
Overhead films
All overhead films must be taken at 110 kVp; suggested films which should be obtained are the following:
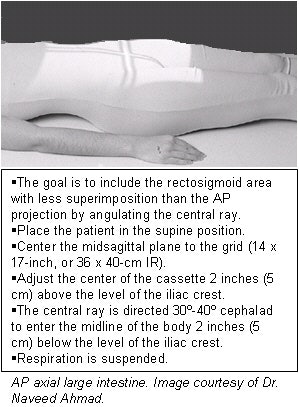
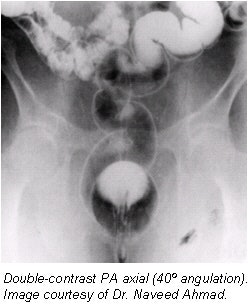
- A posteroanterior (PA) axial projection should include the rectosigmoid area (14 x 17-inch, or 36 x 40-cm IR). The PA projection with the patient in prone projection is preferred over an AP in supine as it results in a more uniform radiographic density of the entire abdomen. The entire colon, including the rectum, should be clearly seen.
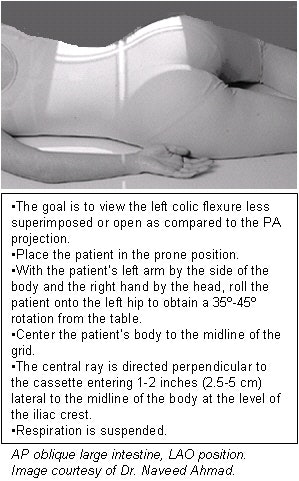
- A PA oblique projection in the left anterior oblique (LAO) position (14 x 17-inch, or 36 x 40-cm IR) should include both flexures.
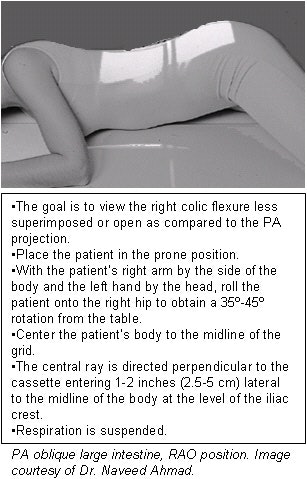
- A PA oblique projection in the right anterior oblique (RAO) position (14 x 17-inch, or 36 x 40 cm-IR) should include both flexures.
- A post-evacuation film. After the radiologist reviews the overhead films, send the patient to the restroom to evacuate as much barium as possible, and obtain an AP abdomen (14 x 17-inch, or 36 x 40-cm IR) post-evacuation film on a horizontal table using 90 kVp.
 |
Patient positioning, imaging techniques for routine double-contrast barium enema
- After insertion of the rectal tube with the patient in the Sims position, tilt the table head down (-30º) and position the patient in the prone position. Release the control clip and fill the colon with barium (105% w/v). Out of 500 cc only 350 cc usually runs into the colon; the remainder of the barium will remain trapped in the tubing.
- Clamp the tubing and elevate the table to the horizontal position. Place the patient in the LPO position and begin slowly inflating the colon with air, using a pneumatic bulb while changing positions to left lateral, LAO, PA, RAO, and right lateral. Slowly administer four or five puffs in each position. When the barium is well in the right colon, stop inflating and position the patient prone.
- Elevate the table to about 80º while the patient is in the PA position. Unclamp the tubing and lower the enema bag to help drain the excess barium.
- Spot films.
- Rectosigmoid colon. After draining the excess barium, turn the table to the horizontal position. Inflate the colon with more air to distend the rectosigmoid colon, then take spot films of:
- Rectum. PA and left lateral.
- Sigmoid. LPO and right lateral.
- Flexures. Elevate the table to the upright (vertical) position and obtain spot film of the splenic flexure (RPO) and the hepatic flexure (LPO).
- Cecum. Decline the table to the horizontal position and obtain AP and LPO views of the cecum. If barium is retained in the cecum, use a lead glove to disperse the barium and turn the patient in LPO or RPO positions.
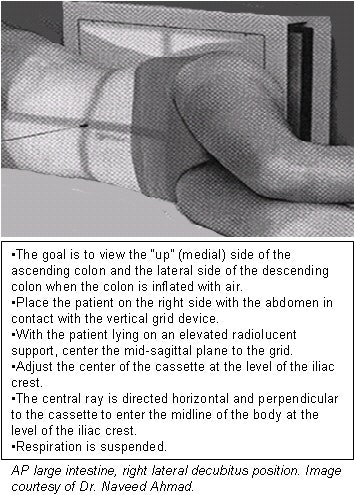
- Overhead films. All overhead films must be taken at 110 kVp; additional air should be insufflated before taking decubitus projections (approximately 5-7 pumps before each decubitus). No post-evacuation film is needed. All overhead films are obtained with the table horizontal. Suggested films that should be obtained are:
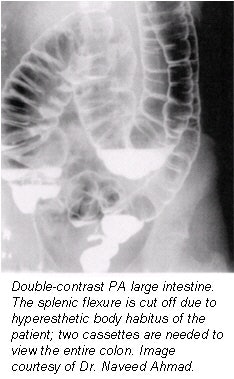
- PA to include rectum (14 x 17-inch, or 36 x 40-cm IR).
- 15º RAO with 35º tube angle caudad for sigmoid (14 x 17-inch, or 36 x 40-cm IR); three overhead films and five on a gurney against an upright bucky.
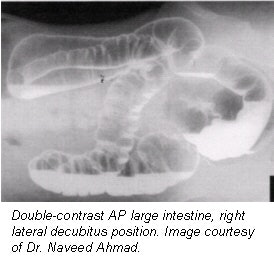
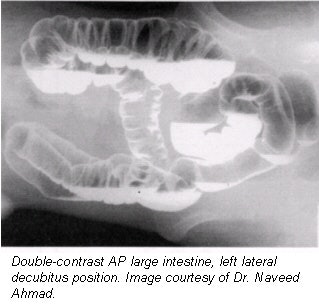
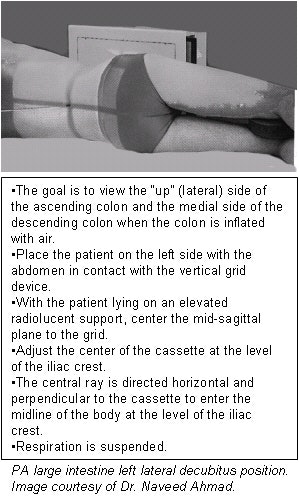
- Left lateral decubitus (14 x 17-inch, or 36 x 40-cm IR).
- Right lateral decubitus (14 x 17-inch, or 36 x 40-cm IR).
- Cross-table lateral rectum with patient prone and tip removed.
- Upright abdomen (14 x 17-inch, or 36 x 40-cm IR).
- The films must be evaluated by a radiologist before the patient leaves the department in case additional radiographs are needed to evaluate suspicious areas. If a lesion is suspected in the distal rectum, removal of the enema tip and additional radiographs will be necessary.
AuntMinnie.com contributing writer
June 27, 2002
Related Reading
Patient positioning tips for a premium UGI series, April 17, 2002
Positioning techniques for quality esophagrams, March 20, 2002
Dorsal and lateral decubitus patient positioning for abdominal x-ray exams, February 28, 2002
AP abdominal projection x-ray positioning techniques, January 16, 2002
Tips and techniques for decubitus and oblique chest x-rays, December 21, 2001
Copyright © 2002 AuntMinnie.com