
The German researchers who pioneered MR colonography (MRC) have been expanding their evaluation of the dark-lumen imaging technique they conceived in 2001. In two newly published articles, the radiologists from University Hospital in Essen discussed the efficacy of dark-lumen imaging, and investigated the effect on the technique of air versus water as a contrast agent.
Before the dark days there was standard MR colonography, which relies on ultrafast T1-weighted 3-D gradient-echo images acquired in a single breathhold on an MR system with high-performance gradients. In standard MRC, the colon is distended with warm tap water mixed with a paramagnetic contrast agent, which renders filling defects as dark masses against the bright colonic lumen.
There is an important limitation to the technique, however, seen in the difficulty of distinguishing stool and small pockets of air from masses and polyps. All are rendered dark on MRI, and in addition, standard MRC requires both prone and supine image acquisition to compensate for the air pockets.
In contrast, so-called dark-lumen MR colonography has proven to be faster and more accurate than the standard bright-lumen technique, the authors wrote in a review article in the Journal of Abdominal Imaging. In dark-lumen MRC, the water-and-paramagnetic-contrast filling agent is discarded in favor of intravenous contrast material that renders the colon bright in contrast to the dark lumen, Dr. Waleed Ajaj, Dr. Jorg Debatin, and Dr. Thomas Lauenstein wrote (Abdominal Imaging online, January 14, 2004).
"Whenever a mass protruding from the colonic wall is detected, the identical part of the colon should be analyzed on the precontrast scan," they wrote. "By measuring signal intensities of the mass in the native and postcontrast scans, a contrast enhancement value can be determined. Hence, the differentiation between small residual stool particles and colorectal lesions is simple: residual stool does not show contrast enhancement, whereas colorectal lesions always do."
The Essen radiologists also have a study in press in which 122 patients were examined with dark-lumen MRC, followed by conventional colonoscopy. MRC visualized no lesions smaller than 5 mm, but correctly detected 16/18 lesions ranging from 5-10 mm in size, Ajai and colleagues wrote in Abdominal Imaging.
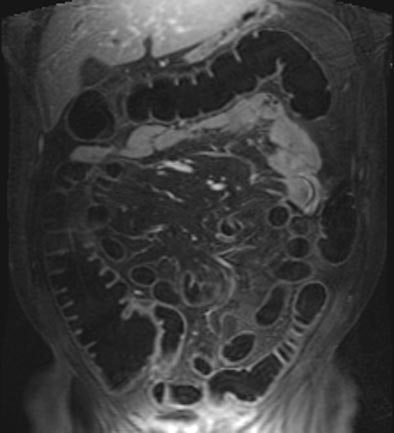 |
| T1-weighted GRE MR colonography images of the same patient. Top: water-filled colon following rectal enema. Bottom: study obtained on another day, following rectal insufflation with room air. Images courtesy of Dr. Thomas Lauenstein. |
 |
According to the results, which are pending publication in Gut, dark-lumen MRC showed no false-positives. MRC also detected inflammatory wall lesions in 25/28 patients, and intestinal fistulae in three patients with Crohn's disease were seen in both modalities, all confirmed on conventional colonoscopy.
Similar accuracy was seen in a 2001 study (Dr. Thomas Lauenstein, Dr. Christoph Herborn et al, Rofo Fortschr Geb Rontgenstr Neuen Bildgeb Verfahr, Sept. 2001, Vol. 173:9, pp. 785-789).
"Both studies emphasize that dark-lumen MRC may overcome several limitations inherent to bright-lumen MRI techniques," the authors wrote in Abdominal Imaging. "The intravenous application of the paramagnetic contrast technique allows the direct depiction of the colorectal wall. Thus, the bright colonic wall can be easily discriminated from the dark, water-filled colonic lumen. This form of direct visualization of all colorectal pathologies reduces the incidence of false-positive findings...."
They cautioned that patients must be carefully screened for contraindications to MRI, including severe claustrophobia, or the presence of metallic implants, cardiac pacemakers, or hip prostheses -- which is not normally a contraindication to MRI, but impedes analysis of the rectum and sigmoid colon.
Comparing air to water contrast in MRC
Another new study by the Essen radiologists sought to determine if either air or water as a colon insufflation agent performed better in dark-lumen MRC (Journal of Magnetic Resonance Imaging, February 2004, Vol. 19:2, pp. 216-221).
"The fear of compromised image quality due to susceptibility artifacts at air/tissue interfaces has long favored the use of water or water-based solutions for colonic distension in MRC," they wrote. "With the availability of high-performance gradients permitting data acquisition with very short echo times, the potential of relevant susceptibility effects is reduced. Accordingly, interest in the use of gaseous agents has grown. They avoid the risk of spillage and have been suggested to be associated with less discomfort compared to fluid."
The group performed dark-lumen MRC followed by conventional colonoscopy on 50 patients suspected of having colorectal pathologies, who were randomized into two groups of 25 patients undergoing either tap water or room-air insufflation prior to imaging. In addition, five healthy volunteers agreed to undergo MRC twice, once with water and once with room air, prior to the conventional exam.
The patients and volunteers underwent standard bowel preparation including 3 L Golytely (Braintree Laboratories, Braintree, MA), and were given 40 mg of Buscopan as an antispasmolytic agent, prior to filling with approximately 2,000 mL of warm tap water or 2,000 mL of room air via a bladder catheter.
MR data were acquired using a combination of two surface coils on a 1.5-tesla Magnetom Sonata scanner (Siemens Medical Solutions, Erlangen, Germany). T1-weighted 3-D gradient-echo images (96 slices, effective slice thickness 1.54 mm) were acquired in the coronal plane, and sequence parameters included TR/TE 3.1/1.1 msec, flip angle 12º, FOV 450 x 450. Then a paramagnetic contrast agent, Gd-BOPTA, was administered intravenously (0.2 mmol/kg) and the same imaging sequence was repeated after a 75-second delay.
The 3-D MRC data, both pre- and post-contrast, were examined on a Siemens Virtuoso workstation by two radiologists who were blinded to the results and who made their diagnoses by consensus. The analysis included calculation of the signal-to-noise ratio between the colonic wall and lumen for each of six colonic segments, grading of distension in each segment, grading for MR artifacts, and assessment of colorectal pathology.
According to the results, water-distended MRC found four masses in four patients (25 mm, 20 mm, 10 mm, and 8 mm) as well as changes compatible with inflammatory bowel disease in another four patients, the authors wrote. The two largest masses were malignant. A single 4-mm polyp was missed on the water-based technique, as confirmed at same-day conventional colonoscopy in all subjects.
The air-insufflated MRC cohort revealed another four masses in four patients, and changes indicative of ulcerative colitis in three. No additional pathologies were found on conventional colonoscopy.
"All detected colorectal masses enhanced after the intravenous administration of paramagnetic contrast," the authors wrote. "Four lesions (three carcinomas and one polyp) revealed contrast enhancement in excess of that seen in the normal colonic wall," while enhancement in the remaining lesions was identical to that of the colonic wall.
The image-quality rating trended better with air distension (1.2 for air versus 1.3 in water among the volunteers), but the difference wasn't statistically significant. However, the use of air produced significantly better colonic distension than water (p<0.05), with a mean rating of 1.07 for air compared to 1.31 for water among the patients.
In patients or volunteers, artifacts were not a problem with either air or water distension, although there were a few artifacts related to motion or wrapping. However, there were statistically significant differences in the contrast-to-noise ratio, with a mean of 43.5 for air distension and a mean of 36.3 (p< 0.05) for water overall. Preferences among the five volunteers were inconclusive: two preferred each method, and one preferred neither.
"Small water spills and one instance of rectal incontinence after (water distension) were offset by two patients complaining about bowel spasms after air insufflation," the authors stated.
The dark-lumen technique overcomes many of the limitations of previous MRC protocols, the authors stated. "The three-dimensional nature of the utilized T1-weighted sequence provides excellent spatial resolution in all three planes, thereby permitting the detection of colorectal masses as small as 5 mm."
Moreover, eight of nine lesions were detected on water-filled MRC, and no lesions were missed when air distension was used. And, they said, the use of ultrashort (0.6-second) echo times virtually eliminated the presence of susceptibility artifacts in the presence of air distension because "there is simply not time for disphasing to occur. Thus it was not surprising that image quality of air- and water-distended datasets did not reveal a statistically significant difference."
"We conclude that MRC...can be performed using either air or water as a distending agent," they wrote. Still, "slightly better CNR and improved distension of the rectum and sigmoid colon seem to favor air distension."
By Eric BarnesAuntMinnie.com staff writer
February 24, 2004
Related Reading
RARE technique shows benefits in MR colonography, July 15, 2003
German group optimizes barium-sulfate tagging in MR colonography, January 22, 2003
German group optimizes barium-sulfate tagging in MR colonography, January 22, 2003
Copyright © 2004 AuntMinnie.com




















