Evidence continues to mount that the link between mental and physical health is an intimate one. While that may seem like a perfectly obvious connection, healthcare professional are not always taking it into account when they treat patients, especially those with heart disease.
According to a new study by psychiatrists from the University of Arizona in Tucson, emotional stress may be a trigger for otherwise unexplained cases of cardiac arrest. On a similar note, investigators from the Ohio State University School of Public Health in Columbus determined that people with heart failure, or those who experience a heart attack, also suffer from psychological distress, yet only about one-third of these patients visit a mental health professional (Psychosomatic Medicine, May-June 2005, Vol. 67:3, pp. 359-365; European Heart Journal, June 9, 2005).
Can mental distress actually bring on coronary artery disease? A multidisciplinary group from the University of Pittsburgh sought to answer that question by taking a closer look at atherosclerosis in depressed women.
"The present study tested the hypothesis that healthy African-American and white, middle-aged women with a history of recurrent major depression have a greater risk of coronary artery and aortic calcification compared with women with a single episode or no history of depression," wrote Patricia Agatista, Ph.D., from the university's department of psychiatry. Her co-authors are from the departments of cardiology, neurosurgery, and epidemiology (Archives of Internal Medicine, June 13, 2005, Vol. 165:11, pp. 1229-1236).
For this research, 58 African Americans and 152 Caucasians were enrolled. They were a subgroup of the Study of Women's Health Across the Nation (SWAN), a multisite, multiethnic, longitudinal study of women's health issues as they transition through menopause. They underwent electron beam tomography (EBT) tests to measure calcification in the coronary arteries and aorta. They also underwent psychological testing with the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders (SCID-IV/NP).
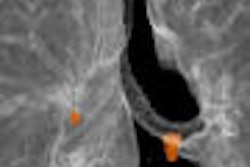
For the scans, the CT unit (C-150 Ultrafast CT, GE Healthcare, Chalfont St.Giles, U.K.) was set in CVA mode so that gating was unnecessary. Three passes were made on EBT to evaluate anatomy, coronary arteries, and the aorta. Calcium scoring was done on a DICOM workstation using software that implemented the Agatston method.
Of the 210 women in this study, 25% met the criteria for history of recurrent major depression. Most of these women were white and perimenopausal. They also had a higher waist-hip ratio, a higher fasting glucose level, and were better educated, the authors reported.
According to the results, any coronary and any aortic calcification were found in 45% of the subjects. Forty-nine women of these women had a coronary calcium score greater than or equal to 10. The aorta calcium score was greater than 100 in 53 women. Elevated depressive symptoms tended to be associated with having any coronary calcification (14.6% of women) versus none (6.5%).
"Women with recurrent depression had more than double the odds of having coronary calcification.... Women with recurrent depression were three times more likely to be in the high aortic calcification group," the authors stated. "The strongest predictors of calcification were (body mass index), waist-hip ratio, HDL-C level, triglyceride level, glucose level, and current smoking status."
Agatista's group suggested several reasons this link may exist between depression and calcification. Depressive behavior may invoke poor dietary habits and a sedentary lifestyle, which contributes to weight gain. In addition, depression can lead to metabolic syndrome, they suggested.
In an accompanying editorial Grant Grissom, Ph.D., and Dr. Robert Phillips, Ph.D., questioned why depression is "not on the radar screens" of physicians, especially if treating the disease means reducing morbidity and morality (Archives of Internal Medicine, June 13, 2005, Vol. 165:11, pp. 1214-1216).
"Depression screening is justified by its consistently documented impact on quality of life, even in the absence of cardiac benefit," they wrote.
By Shalmali Pal
AuntMinnie.com staff writer
June 24, 2005
Related Reading
Enlarged heart more common in blacks than whites, June 7, 2005
Canadian cardiologists define low risk for women with chest pain, May 30, 2005
Imaging tackles cardiac 'octopus pot' syndrome, April 19, 2005
As cardiac CT interest heats up, so does EBCT, MDCT debate, March 31, 2005
Copyright © 2005 AuntMinnie.com