In female breast cancer patients, interval follow-up imaging rather than imaging workup or biopsy should be performed for hepatic lesions that are "too small to characterize" (TSTC) on CT. More so if it is stage 0 breast cancer and there are no clinical findings supporting suspicion of liver metastasis, according to recommendations by researchers from the Memorial Sloan-Kettering Cancer Center in New York City.
The recommendations are based on the findings of a retrospective study at the institution that showed that in as many as 96.9% of cases in which there was no definite liver metastasis and the hepatic lesions were deemed TSTC, the lesions were benign.
The study population included 1,012 women diagnosed with breast cancer and who underwent contrast-enhanced CT, including liver exam, at the Memorial Sloan-Kettering Cancer Center between 1998 and 2002. In this patient group, 277 women without liver metastasis or with indeterminate findings for liver metastasis had one or more hepatic lesions deemed TSTC.
Records of follow-up imaging that include at least one CT, MRI, or US exam were available for 191 patients, and the researchers reviewed these records for changes in lesion size to evaluate the prevalence and clinical importance of TSTC hepatic lesions. If lesion size had changed, the medical records and images were reviewed.
"Results of best- and worst-case analyses showed that the lesions were benign in 96.9% (95% CI: 93%, 99%) and 92.7% (95% CI: 88%, 96%) of women, respectively," the researchers wrote in Radiology (June 2005, Vol. 235:3, pp. 872-878).
"These worse- and best-case estimates were needed owing to the lack of a reference standard for some of the lesions, such as those that were not visible at follow-up imaging," they added.
For the best-case analysis, lesions were considered benign in 175 patients who showed no change in lesion size, and in 10 other patients. For the worst-case analysis, lesions in the 175 patients and two other patients were considered benign. Of these two cases, lesions were shown to represent cysts in one patient, and in the other the lesion was not seen on MR imaging.
Of the eight patients included in the best-case analysis and excluded from the worst-case analysis, lesions were not visible on follow-up imaging in five. In three women who had lesions that were not visible and were undergoing adjuvant chemotherapy, the lesions were considered benign based on the clinical context by the treating physicians. For one woman the lesion was considered likely an artifact at initial CT, and in another woman the lesion was not likely visible due to lack of intravenous contrast material at follow-up CT.
 |
| Transverse contrast-enhanced helical CT scans of the abdomen in a 70-year-old woman with infiltrating ductal carcinoma (stage IIA at initial presentation) and hepatic cysts. Above, baseline scan obtained with 7-mm-thick sections shows a hepatic lesion (arrow) deemed TSTC. Below, follow-up scan obtained with 7.5-mm-thick sections 11 months later shows that the hepatic lesion (arrow) has increased in size -- from 17 x 10 mm to 20 x 10 mm. A second hepatic lesion (not shown) showed a similar increase in size -- from 3 x 3 mm to 5 x 5 mm. Subsequent MR imaging of the abdomen revealed the presence of hepatic cysts, but no hepatic metastasis. Figure 3AB, Hanan KI, Patterson SA, Panicek DM, "Hepatic Lesions Deemed Too Small to Characterize at CT: Prevalence and Importance in Women with Breast Cancer," Radiology 2005; 235:872-878. |
 |
Among the three other patients included for the best-case analysis and excluded for the worst-case analysis, the lesion was enlarged slightly but of indeterminate etiology in one patient, and in two patients the change in size was indeterminate because development of hepatic metastasis obscured the original lesion.
"Although metastatic disease is the greatest clinical concern when at least one hepatic lesion deemed TSTC is demonstrated at CT, those lesions could also be due to various other entities, such as cysts, biliary hamartomas, and hemangiomas," the research group stated.
Overall, lesions were no longer visible on follow-up imaging in eight patients, enlarged in six, and unchanged in 175. Among the enlarged lesions, lesions showed typical features of metastasis in two patients, and in one patient CT-guided fine-needle aspiration showed metastasis from the patient's known pancreatic cancer.
"Breast cancer does not preclude one from having other cancers, and this patient is a reminder of that important fact," the group wrote.
A hepatic lesion was deemed TSTC if it was 1.5 cm in diameter or smaller, or if the interpreting radiologist determined it was too small to allow accurate characterization on available images. Imaging was done on a conventional nonhelical scanner and helical scanners with one to 16 detector rows (GE Healthcare, Chalfont St. Giles, U.K.).
Section thickness was 7-7.5 mm, the range used for standard protocols to survey the body for metastasis at the institution. "If thinner sections were used, it is likely that some lesions would have been characterized as cysts or hemangiomas and that additional, smaller hepatic lesions deemed TSTC would have been discovered," the authors wrote.
The decision to provide follow-up imaging or immediate further workup must be made depending on the clinical scenario, including histologic type and initial stage of breast cancer, results of liver function tests, and the presence of symptoms or signs indicating possible hepatic metastasis, the group recommended.
"Even when a hepatic lesion deemed TSTC cannot be confidently characterized at imaging, interval follow-up CT, MR imaging, or US can be useful for assessing a change in lesion size; for all practical purposes, those small hepatic lesions that remain stable over time are assumed by the treating physician to be benign," the researchers concluded.
By N. Shivapriya
AuntMinnie.com contributing writer
July 11, 2005
Related Reading
MRI after CT cuts need for liver biopsies in cancer patients, May 19, 2005
Concentrated contrast improves liver lesion conspicuity, May 16, 2005
Contrast MR shows gains in preoperative liver lesion depiction, September 29, 2004
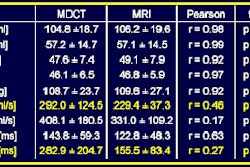
Multiphasic MDCT with contrast boosts liver, urography results, March 1, 2004
Ultrasound effective in diagnosis, treatment of cystic liver lesions, May 15, 2003
Copyright © 2005 AuntMinnie.com