Once the tumor is resected, there's no way of knowing whether rectal cancer surgery will be curative. But there is an excellent way to monitor patients for recurrence, according to researchers from Taiwan.
In a recently published study that followed 434 rectal cancer patients with virtual colonoscopy and colonoscopy, the team from Chang Gung Memorial Hospital in Taipei found that VC was 100% sensitive for detecting recurrent cancer, catching a few cases that were negative or indeterminate on optical colonoscopy, but also producing a few indeterminate results that were in fact negative.
Overall, VC's ability to detect endoscopically obscure recurrences offers important advantages over both endoscopy and abdominal CT, the group stated, making it an ideal test for the frequent follow-up these patients need after surgery.
"Approximately 70% of colorectal cancers can undergo potentially curative resection. Unfortunately, colorectal cancer recurs in 30% of these patients," wrote Drs. Yau-Tong You, Chung-Rong Chang Chien, Jeng-Yi Wang, and colleagues in the World Journal of Gastroenterology. "If radical resection of local recurrent cancer is performed before distant metastatic or unresectable disease develops, one-third of patients can increase their survival time" (WJG, January 2006, Vol. 7:12, pp. 123-126).
The study began with 434 patients from 2000-2004 who underwent potentially curative resection for invasive rectal cancer (181 stage B and 253 stage C). Eighty of the patients (43 men and 37 women ages 28-82; average 64 years) underwent surveillance with both colonoscopy and virtual colonoscopy from 20 to 55 months. The average time between surgery and same-day colonoscopy and VC was 32 months (range of 20-55 months).
A day before CT imaging, patients underwent a standard bowel cleansing with polyethylene glycol and 25-mg bisacodyl tablets. Before the exam, they were given 20 mg of IV hyoscine butylbromide (Buscopan, Boehringer Ingelheim, Ingelheim, Germany) as an antispasmodic. Manual room-air insufflation with a rectal tube was used to distend the colon to patient tolerance. The adequacy of distension was monitored with scout images, and the volume of insufflated air measured 1,500-2,000 cm2, followed by additional insufflation if needed.
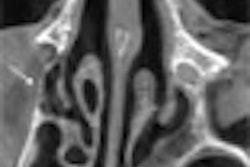
Seventy seconds following contrast administration of 150 mL of Isovue 300 (Bracco, Milan, Italy) at 3-5 mL/sec, patients underwent prone and supine imaging on a LightSpeed Plus and LightSpeed QX/i scanner (GE Healthcare, Chalfont St. Giles, U.K.). The protocol included 5-mm collimation, overlapping 2.5-mm reconstructions, 230-260 mAs, and 120 kVp. An experienced gastrointestinal radiologist examined all data using 2D axial images and 3D endoluminal views with the aid of a GE Sun Advantage Windows and Navigator software, rating local recurrence as either present, absent, or indeterminate. Conventional colonoscopy was performed after VC and there were no complications.
Surgical results showed local recurrence in 51 of 80 patients. Of the 80 patients, 75 had adequate bowel distension, two had inadequate transverse colon distension, and three had inadequate sigmoid colon distension, according to the authors.
"In contrast-enhanced (VC), the five patients showing thickened segmental colon wall and external luminal tumor mass compression were classified as present local recurrence," the authors wrote. "The colonoscopic findings in these corresponding regions showed lumen stenosis, but no mass or mucosal lesions were found in the lumen in all five patients. All five patients received laparotomy for local recurrence based on a clinical presentation of the three abdominal palpable masses and colon obstructions."
Five patients classified as indeterminate on VC underwent additional colonoscopic and VC follow-up several months later; no local recurrence or metastases were found.
"Twenty-three patients whose contrast-enhanced (VC) did not show local recurrence were negative for colonoscopy," and were routinely followed up, You and colleagues wrote. "There was no ... false-negative local recurrent cancer on contrast-enhanced (VC). However, the five patients classified as indeterminate for local recurrence in contrast-enhanced (VC) reports were false-positive." Thus, VC "had a sensitivity of 100%, a specificity of 83%, and an overall accuracy of 94% in detecting local recurrent colorectal cancer."
Although conventional colonoscopy can readily detect intraluminal local recurrence, some local recurrences are not intraluminal and are endoscopically obscure, the group wrote. And while abdominal CT can detect hepatic and peritoneal metastases, it is unreliable for detecting local recurrence except in patients with a previous abdominoperineal resection.
"Unlike these two tests, contrast-enhanced (VC) directly displays the anastomosis, luminal surface, colon wall, and pericolonic tissues," they wrote. "It has, therefore, a potential to detect mucosal, intramural, and extracolonic local recurrences. In our study, the overall accuracy was 94%, which is similar to that in the study by Fletcher et al (AJR, February 2002, Vol. 178:2, pp. 283-290). At the same time, it is also advantageous over the colonoscopy for detecting extracolonic local recurrence and peritoneal metastasis."
In all, 46 of 51 local recurrences developed from the extraluminal soft tissue and local lymph nodes. Forty of these cases were rectal cancer and 47 were stage C at their original primary cancer, which may be related to the high local recurrent rate of the samples.
"As shown in our study, five of the 51 patients (10%) who had local recurrence detected by contrast-enhanced (VC) had no intraluminal recurrence by colonoscopic examination," the authors wrote. In any case, all five underwent laparotomy based on local recurrence of abdominal obstruction, and extraluminal recurrence with or without peritoneal metastasis was found at surgery, they noted.
"Contrast-enhanced (VC) has several advantages over alternative tests in detecting local recurrent colorectal cancer," You et al wrote. "It can be a very helpful adjuvant method to colonoscopy in detecting extraluminal local recurrence, peritoneal carcinomatosis, and distant metastasis. With regard to the threat of colorectal cancer and the early detection of local recurrence and distant metastasis in patients who have undergone potentially curative colonic resections for invasive colorectal cancers, conventional colonoscopy and contrast-enhanced (VC) can complement each other."
By Eric Barnes
AuntMinie.com staff writer
March 8, 2006
Related Reading
Intensive monitoring improves outcome of resected colorectal cancer, February 7, 2006
High magnesium intake lowers colon cancer risk in women, February 6, 2006
Tumor regression after chemoradiotherapy predicts rectal cancer outcome, January 16, 2006
Matrilysin points to colorectal cancer metastatic potential, December 5, 2005
Combined PET/CT accurately detects pelvic recurrence of rectal cancer, September 8, 2004
Copyright © 2006 AuntMinnie.com