Noninvasive cardiac imaging modalities, especially CT and MRI, have transformed the face of cardiac imaging in recent years, challenging the gold standard angiography for accuracy, and opening up an all-but-limitless future for detecting and managing heart disease.
But in the long run, radiologists cannot succeed without formal and significant ties to cardiologists -- and even that might not be enough -- warned Dr. Gabriel Krestin, Ph.D., in a recent talk in Vienna. For one thing piles of money are at stake. And cardiologists still control the patients.
Krestin, who is professor and chairman of radiology at Erasmus Medical University in Rotterdam, Netherlands, and a permanent visiting associate professor of radiology at Stanford University in California, presented the Sir Peter Mansfield honorary lecture at last month's 2006 European Congress of Radiology (ECR).
To begin, radiologists must adopt a more patient-centered approach to healthcare and boost their clinical knowledge, technical expertise, and advanced interpretation skills within the global context of health management, he said.
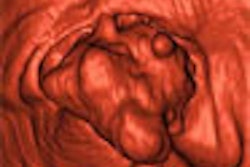
"For us radiologists, imaging of the beating heart may be something of a Holy Grail, not only because the heart is such an important organ, but (because it is) also a very difficult organ in imaging," Krestin said. "This dream is now almost within our grasp, thanks to unprecedented technical developments in recent years."
Some of these techniques are already implemented as part of the clinical armament used for diagnostic decision-making, such as coronary calcium scoring, functional exams in congenital heart disease and left ventricular failure, myocardium viability studies, and coronary CT angiography (CTA), he said.
Further impressive developments lurk just around the corner from clinical utilization. Poised to enter the scene are assessments of total coronary plaque load, characterization of plaque composition, detection of vulnerable plaques, and combined functional and metabolic examinations, Krestin said.
"These exciting achievements have pushed back the frontiers of noninvasive diagnosis of cardiac disease, and expanded the role of the radiologist beyond our traditional turf," he said. But whether this technology will ultimately be a friend or foe to radiologists remains to be seen.
Noninvasive modalities transform cardiac imaging
In a sense, MRI is similar to echocardiography in that it allows interactive imaging of the heart. The operator chooses the signal intensity, contrast, and planes of imaging.
Recent advances have come in the form of new contrast agents, the development of pulse sequences such as steady-state free-precession, respiratory gating techniques, and the use of MR fluoroscopy with more computing power, "allowing not only acquisition in a single heartbeat but during free breathing," Krestin said.
"Today's cardiac toolbox contains a lot of possibilities for imaging the morphology of the myocardium and the great vessels surrounding the heart," he said, either in high resolution or even in four dimensions -- three of space and one for temporal.
Functionally, the contractility of the myocardium can be assessed, and first-pass MRI after contrast administration can show myocardial perfusion. Flow can be quantified and myocardial viability assessed in late-enhancing image data, most strikingly in infarcted areas.
MRI can image the coronary vessels as well, of course, but with important limitations. For example, Krestin noted, a 2001 study by Kim et al found both sensitivity and a negative predictive value of about 80% for coronary artery disease -- and 16% of the segments couldn't be evaluated. And MRI can't see calcium. Fortunately, the coronary vessels is where CT angiography excels.
"We can also evaluate left ventricular contractility with CT, but imaging the coronary arteries is the most ... valuable advantage of CTA," he said. "Coronary artery anomalies can be imaged with great detail, but also stenotic lesions or coronary arteries can be assessed with great accuracy. We can even characterize the plaques leading to such lesions, and classify them as calcific or noncalcific -- or even fibrotic and lipid-containing plaques. We can also evaluate the patency of stents."
And with 15- to 20-second acquisition times in the fastest scanners, CTA is not only improving patient comfort but patient throughput as well.
An upcoming study by Mollet et al will show the strengths and weaknesses of cardiac modalities in a clinical context, Krestin said. The group examined 62 patients with a high pretest probability of coronary artery disease who underwent stress ECG tests, which yielded positive, negative, and in some cases indeterminate results.
All underwent CTA as well as conventional catheter angiography. CTA was positive in many cases in which stress testing was negative or indeterminate, "showing that the stress test has limited specificity and sensitivity," he said. Moreover, multidetector-row CT yielded a 100% negative predictive value. "So if we don't see (the pathology on CT), we can be quite sure the patient has no coronary artery disease," Krestin said.
Krestin cited a case of a 36-year-old smoker with a history of myocardial infarction who developed a new episode of unstable angina two weeks later. Coronary angiography showed no accessible alteration, but 64-slice CTA revealed a slight anomaly of the left anterior descending artery wall. The finding was diagnosed as an eccentric noncalcified plaque on a curved planar reformat, and the finding was confirmed on intravascular ultrasound.
"This shows that we can start to doubt whether catheter coronary angiography is still the gold standard," he said.
More marvels ahead
New MRI pulse sequences include high-diffusion tensor imaging, which can depict myocardial fibers, Krestin said. Image reconstruction hardware continues to advance. Advanced tagging methods combined with prolonged relaxation times allow radiologists to evaluate strain in the myocardium. Molecular imaging modalities are coming online as well.
High-field MRI is improving signal-to-noise ratios and visualization of the myocardium as well as the coronary arteries, yet at a cost of increased specific absorption rates (SAR). Researchers are also combining cell tagging with high-resolution MR images.
"We can visualize the (superparamagnetic iron oxide particles or SPIOs) surrounding the nucleus," he said of a sample image.
"These high-resolution images show a single myoblast with resolution of 20 x 20 microns produced on a clinical magnet. The cells can be injected into myocardium ... replacing areas of myocardial infarction. This can be used already. And with imaging we can prove that the cells that are labeled are really there where we expect them to be."
Meanwhile, CT is moving ahead with ever more detector rows, increased coverage, and faster acquisition with dual-source systems. Flat-panel detectors offer the possibility of increased spatial resolution, although this is still quite slow, Krestin said. PET/CT is successfully combining metabolic and anatomical information.
Who's doing the research?
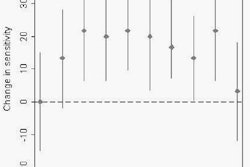
It's not radiologists. Krestin and colleagues performed a Medline search of cardiac CT studies over the past 10 years, and found that nonradiologists are performing more studies than radiologists. The disparity is even more pronounced in MRI. "Particularly in the last two years, nonradiologists are publishing almost twice as much as radiologists," he said.
There is tremendous interest in noninvasive cardiac imaging in the media worldwide, and the vast amount of money at stake guarantees there will be plenty of competition. An estimated 1.8 to 2.4 million cardiac imaging procedures are being performed in Europe each year at a cost of some 1.5 to 2.5 billion euros, Krestin said.
Showing them the money
"Will we (radiologists) become rich? There are some doubts about that," Krestin said. "The former president of the ACC (American College of Cardiology) says they will fight for imaging services, and they are convinced that they will win. If we learn from the history of how we lost coronary angiography, then maybe history is repeating itself."
An example came from Dr. David Levin and colleagues from Thomas Jefferson University in Philadelphia, who reported from 1998 Medicare data that radiologists conducted just 16.7% of all noninvasive cardiovascular imaging, whereas cardiologists conducted 61.5%, surgeons 4.8%, and other physicians 16.9% of the examinations. Echocardiography accounted for 63.4% of all exams (American Journal of Roentgenology, February 2002, Vol. 178:2, pp. 303-306).
In the next round, noninvasive cardiac imaging, radiologists may once again prove too passive or uninterested to take on the imaging exams and the research that must accompany them, Krestin said.
"Can we expect to take over those 2.5 billion euros from the cardiologists and (that) they will permit it? The imaging methods were all first developed by radiologists, but cardiologists took them over over the years," Krestin said. "Technical competence is claimed by radiologists, but cardiologists are clinical experts and they understand cardiac results, and ... definitely cardiologists control the patients, so we might learn from history."
Ties that bind
"Teamwork is essential for realizing the potential of a growing market," Krestin said. His group in Rotterdam, for example, formalized cooperation with cardiology by setting up a cardiac imaging section embedded within the cardiology and radiology departments, even setting up joint patient appointments. The personnel and technical equipment costs of exams are reimbursed at cost, and all research output -- some 70 papers so far -- is published under dual affiliation, he said.
"Noninvasive cardiac imaging is a highly exciting field of application for CT and MRI," Krestin concluded, adding that technological development is far from complete.
"Cardiac imaging necessitates the most advanced technology developed, so if we (radiologists) don't participate, we'll miss the contact with these developments," he said.
"Radiologists have to get involved in cardiac imaging -- no doubt about that," he said. "The highest standards of education and examination are required. Radiologists must also participate in clinical and basic research, however. The turf battle will be fierce -- and it is not obvious that we will win."
And if radiologists are to remain competitive, they'll need to formalize cooperative ties with cardiologists as soon as possible -- and it may already be too late, Krestin said. The take-home message for now is teamwork, he said, "and maybe you will win afterwards."
By Eric Barnes
AuntMinnie.com staff writer
April 10, 2006
Related Reading
Interventional radiology needs rebranding, revitalizing, March 7, 2006
Radiologists maintain dominance in breast biopsy procedures, January 10, 2006
Radiologists retain MRI turf, for now, December 1, 2005
Radiologists nab share of Medicare bone scan market, September 12, 2005
Turf sharing: Rads and cards in joint venture imaging, July 28, 2005
Copyright © 2006 AuntMinnie.com