Wrist injuries are quite commonplace, but there doesn't seem to be a common imaging protocol in place for assessing scaphoid fractures, according to an international survey conducted by U.K. researchers. And, despite the need for diagnostic urgency, the timing of wrist imaging exams is not set in stone.
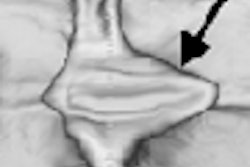
Multiple modalities can be used to assess these fractures -- scintigraphy, CT, sonography, MR -- and all have their pros and cons, wrote Dr. Ashley Groves and colleagues in the American Journal of Roentgenology. Groves' group is from the Institute of Nuclear Medicine at University College in London and from Addenbrooke's Hospital at Cambridge University.
Depending on which side of the pond you are on, recommendations for the most effective protocol differ: the American College of Radiology considers MRI and x-ray to be the most appropriate imaging tools in scaphoid fractures, but does not back scintigraphy. The Royal College of Radiology promotes MRI, CT, and scintigraphy equally when x-ray is negative.
For this survey, the authors polled physicians at 200 hospitals on six continents. Countries included in the survey were Australia, Canada, Germany, India, the Netherlands, Saudi Arabia, and the U.S. Of the 200 hospitals, 105 (88 university hospitals) answered the survey for a response rate of 52.5%. Nearly all of the respondents (95.2%) were imaging specialists.
According to the survey results, only 6.7% of those who responded shared identical scaphoid imaging strategies. Of the 105 institutions, most (78.1%) did not have a fixed imaging protocol.
The most common protocol was four x-ray views, repeated at 10 to 14 days, followed by MRI. Almost 30% of those surveyed said that MRI was the definitive investigative imaging tool, followed by CT (18.1%), and scintigraphy (13.3%).
The authors pointed out that in Europe, CT was the most commonly used second-line investigation, even though the sensitivity of the modality in this setting has been questioned. On the other hand, scintigraphy was the more popular option in Australia and Asia, despite the fact that the modality is limited in resolution and specificity. Finally, MRI was more often used in nonuniversity hospitals.
"The extent of variation in practice probably also reflects deficiency in scientific evidence regarding best practice in the imaging scaphoid trauma," the authors wrote (AJR, December 2006, Vol. 187:12, pp. 1453-1456).
The authors also found wide variation in the timing of the imaging, with 59 respondents citing a 10- to 14-day delay between initial and second-line exams. "The rationale for performing delayed imaging is controversial," the authors explained. Reasons for delayed imaging included time to allow symptoms to subside and fracture widening for better radiographic identification.
By Shalmali Pal
AuntMinnie.com staff writer
December 18, 2006
Related Reading
Part I: Choosing between MR and US in musculoskeletal imaging, September 7, 2006
Color Doppler US shines for carpal tunnel syndrome, May 18, 2006
MDCT, scintigraphy yield very different reads on wrist fractures, May 18, 2005
Copyright © 2006 AuntMinnie.com