Excessive weight and a high body mass index (BMI) pose a host of complications in breast cancer patients. Overweight women who undergo axillary lymph node dissection are more likely to develop lymphedema. In addition, BMI and breast size affect the rate of intraoperative sentinel lymph node identification. Finally, the inability of adipose tissue to pick up blue dye means nodal hot spots may be missed by planar imaging.
Nuclear medicine specialists have proposed using SPECT/CT in overweight breast cancer patients to improve sentinel node identification. Advantages of the hybrid modality include improved spatial resolution, image quality, and attenuation correction, wrote Dr. Hedva Lerman and colleagues in the Journal of Nuclear Medicine. Lerman's group is from the Tel-Aviv Sourasky Medical Center and Tel-Aviv University in Israel, as well as the Haifa office of GE Healthcare.
For this study, planar imaging and SPECT/CT exams were done in 220 women with invasive breast cancer, including 140 with palpable masses. Those with a BMI value of 25-29.9 kg/m² were considered overweight; those with a BMI of 30 kg/m² or more were considered obese. Of the 220 women, 122 were overweight or obese.
Prior to surgery, a 74 MBq dose of technetium-99m rhenium colloid was injected into three different sites, depending on the presence and number of masses: peritumoral sites, sites along the biopsy cavity border, and periareolar sites. Planar imaging was done until hot nodes were identified, up to 24 hours after injection. For SPECT, a dual-head gamma camera was used while the CT scanner was set at 140 kVp and up to 2.5 mAs (Hawkeye or Infinia Hawkeye, GE Healthcare, Chalfont St. Giles, U.K).
Two nuclear medicine physicians interpreted all lymphoscintigraphy exams in addition to classifying hot nodes on the SPECT/CT images. Imaging results were correlated with BMI, detection of sentinel nodes, blue dye detection, and histology.
According to the results, adding SPECT/CT improved the identification of hot nodes in overweight and obese patients. SPECT/CT found hot nodes in all 220 patients including 29 with a BMI of 28.38 kg/m². In comparison, planar imaging failed to find hot nodes in 49 patients with the same BMI. Also, SPECT/CT detected hot nodes in 109 patients (89%) with a BMI of 30 kg/m², including 18 out of 34 with negative planar imaging results.
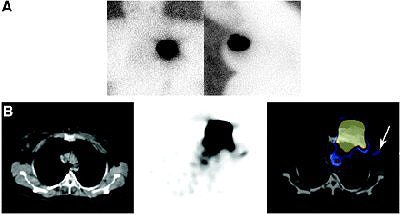 |
| Negative planar imaging and positive SPECT/CT identification of hot node in 64-year-old overweight patient (BMI, 29.1 kg/m²). (A) Anterior and left lateral planar images of chest obtained with 57Co flood. Except for uptake at injection site, no hot spot was identified. (B) SPECT/CT transaxial images. CT, SPECT, and fused images are shown from left to right. Hot node was detected at level I of left axilla (arrow), in keeping with SN. Increased uptake detected in left mediastinum appears to be non-nodal uptake in blood vessel. Copyright © by the Society of Nuclear Medicine Inc. |
"Both SPECT and attenuation correction were found to contribute to better identification of hot nodes by SPECT/CT than by planar imaging," the authors wrote. "The superiority of SPECT/CT appears to be enhanced in overweight and obese patients. Although in planar imaging there is a progressively declining rate of detection as the BMI increases, the rate of detection by SPECT/CT is relatively stable" (JNM, February 2007, Vol. 48:2, pp. 201-206).
Other overall results: SPECT/CT found 402 hot nodes in 200 patients and was the sole modality to detect nodes in 59% of the patients who had negative planar imaging results. The 85 hot nodes detected with SPECT/CT alone included nodes revealed by better spatial resolution. The detection rate for planar imaging in all patients was 78% versus 91% for SPECT/CT. For the patients in whom the blue dye technique failed, SPECT/CT found sentinel nodes in 36 patients.
The authors acknowledged that the rate of false-negative SPECT/CT results was higher in their study than in previous ones (11%), but the modality "identified hot nodes in 18 additional patients and had a statistically higher rate of detection of hot nodes in overweight patients."
They also pointed out that the surgeons opted to perform procedures based solely on the SPECT/CT results in the overweight and obese patients. "The assessment of lymph node involvement is a major prognostic factor in patients with breast cancer," the group wrote. "Thus, early and accurate identification of lymph node involvement enables adequate therapeutic decisions.... The 3-dimensional data of fused SPECT/CT images have greater clinical relevance."
By Shalmali Pal
AuntMinnie.com staff writer
February 14, 2007
Related Reading
Timing of weight gain affects breast cancer risk, December 27, 2006
SLN procedure in pregnant breast cancer patients leads to negligible fetal dose, August 14, 2006
Intradermal injection for breast scintigraphy allows direct access to swollen nodes, May 10, 2006
Copyright © 2007 AuntMinnie.com