Step-and-shoot image acquisition is stepping up to the plate and shooting down other dose-reduction techniques for coronary CT angiography (CCTA).
In an important new study from Virginia, radiologists compared standard retrospectively gated CCTA to the new prospectively gated technique, and achieved dose reductions of up to 83% with the new method -- all without loss of image quality or diagnostic utility. In fact, both of these measures were slightly higher using step-and-shoot.
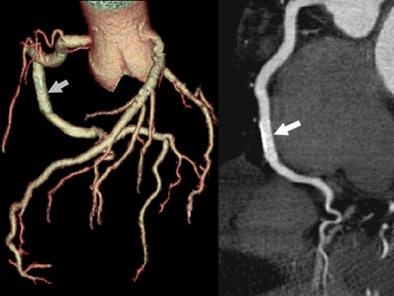 |
| A 55-year-old man presented with chest pain and history of a 3-year-old right coronary artery (RCA) stent. CTA effective dose using prospectively gated axial (PGA) technique was 0.90 mSv. Volume-rendered image of the coronary tree left depicts the stent (arrow) and many side branches. On the right a curved multiplanar reformatted image of the RCA depicts a widely patent 3.0-mm drug-eluting stent (arrow). |
Attempts to cut the CCTA dose by lowering mAs or kVp have been far less successful, impacting radiologists' ability to read the exams.
The study, presented at the 2006 RSNA meeting in Chicago, represents the first clinical validation of Hsieh et al's step-and-shoot imaging method, which was presented at the 2005 RSNA meeting as a hot topic, and later published in Medical Physics (November 2006, Vol. 33:11, pp. 4236-4248).
"We have all had some trouble with the relatively high doses associated with CCTA studies, especially at 64-row MDCT, where the dose is significantly higher than at 16-row MDCT," wrote principal investigator Dr. James Earls in an e-mail to AuntMinnie.com.
Step-and-shoot CCTA could potentially eliminate a principal drawback of retrospectively gated 64-slice CCTA -- with its mammoth radiation dose averaging 10-25 mSv per exam -- in effect lowering the bar for ordering CCTA instead of invasive angiography, and potentially hastening clinical adoption of the scans.
"While all patients will benefit from lowering the effective dose of CCTA exams, we feel this is especially promising for those at higher risk for radiation-induced malignancies," Earls wrote. "These would include premenopausal women because of direct breast exposure, and younger patients as a whole because of the longer lag time that exists for cancers to develop."
The study was performed by Earls and his co-authors Dr. Elise Berman; Dr. Charlene Curry; Dr. Bruce Urban; Colin McCulloch, Ph.D.; Judy Lane; and Robert Jennings from Fairfax Radiological Consultants in Fairfax, VA, and Inova Fairfax Hospital in Falls Church, VA.
They evaluated multiple measures of image quality including enhancement characteristics, reliability, and absorbed radiation dose of CCTA using adaptive prospectively gated axial (PGA) CT, which offers a significantly lower dose compared to retrospectively gated helical (RGH) CT.
The current standard for CCTA is an RGH technique in which the patient and table move through the gantry at a steady speed. A low pitch of 0.2 to 0.4 is needed to cover the entire cardiac volume, especially to compensate for any ectopic beats, which can result in misregistration and gaps in coverage, the authors explained. Thus, the same anatomy can be exposed to the x-ray beam as many as four or five times to ensure coverage, raising the cumulative radiation dose.
In contrast, the step-and-shoot method significantly reduces exposure of the anatomy to multiple passes of the x-ray beam, in part by predicting heart rate variability rather than overscanning to compensate for it.
A complementary reconstruction algorithm developed by Hsieh et al overcomes the longitudinal truncation problem resulting from the conebeam geometry, resulting in minimal overlap of anatomic coverage between scans while providing robust ECG gating, the authors explained.
The table is stationary during PGA image acquisition, then moves to the next location for another scan that is initiated by the next normal cardiac cycle. The incrementally moving table permits adaptive ECG triggering, Earls explained. The method takes advantage of the large 40-mm (64 x 0.625-mm) volume coverage available on 64-detector MDCT that enables complete coverage in the heart in two to four steps.
The study included 203 CCTA exams, including 82 imaged with routine RGH CT, and 121 scans utilizing the PGA technique. The PGA group included 71 men and 50 women (mean age 56.7, mean BMI 28.32), while the RGH group included 44 men and 38 women (mean age 55.6, mean BMI 27.62).
There was little difference between the two groups, Earls wrote. "We saw no difference in the heart rate, age, BMI, or sex distribution."
The patients were given a beta-blocker (50-100 mg of metropolol) if resting heart rate exceeded 60 beats per minute (bpm), supplemented when necessary with 5 mg of intravenous aliquots of metropolol every five minutes to a maximum dose of 20 mg. Eighty-seven percent of the RGH patients received a beta-blockade compared to 91% of the PGA group.
All images were acquired on a 64-slice CT scanner (LightSpeed VCT XT, GE Healthcare, Chalfont St. Giles, U.K.) using software version 06MW34.3b. Both methods used a rotation time of 350 msec, temporal resolution of 175 msec, detector aperture of 0.625 mm, scan field-of-view of 25 cm, and tube voltage of 120 kVp. The radiologists, all highly experienced in CTA acquisition and interpretation, acquired scout images, a low-dose calcium scoring scan, test bolus scan, and a CT coronary angiogram.
Sequential scans were performed every two seconds for 30 seconds after administration of a test bolus of 20 mL of iodixanol 320 (Visipaque, GE Healthcare) at 5.5 mL/sec in a craniocaudal direction, according to the authors. The main contrast injection (50-80 mL of iodixanol 320 at 5.5 mL/sec) was determined by the time to peak enhancement from the test bolus plus four seconds.
For the standard RGH acquisitions, mAs ranged from 349-771 (mean 647) depending on BMI and chest circumference; for the PGA studies, the range was 300-800 (mean 508). Reconstruction phases of 5% to 95% were used in the RGH images, with reconstruction as available in the PGA images.
The team used a new GE software application (Snapshot Pulse) that has received U.S. Food and Drug Administration 510(k) clearance for body scanning, and will be in wide clinical release in 2007, according to the authors. One drawback, however, is that the current software supports only single-sector reconstruction, and for this reason the team set an upper limit of 70 bpm as a contraindication to PGA imaging.
The PGA scans were acquired using three to five incremental 64 x 0.625-mm image groups, requiring two to four incremental table translations of 35 mm with a 5-mm overlap between successive 64-slice groups, the authors wrote. The effective temporal resolution was 175 msec with halfscan weighting.
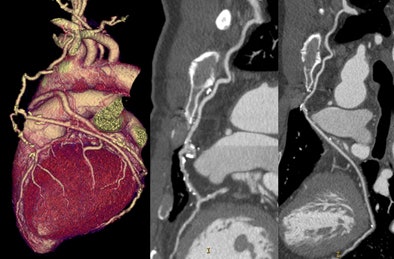 |
| A 47-year-old man with new chest pain five years after coronary artery bypass grafting (CABG). CTA effective dose using PGA technique was 3.87 mSv. Volume-rendered view of the heart depicts a complex bifurcated left internal mammary artery (LIMA) graft. The LIMA is anastomosed to the left anterior descending (LAD) coronary artery (center) and a radial artery branch connects the mid-LIMA to the second obtuse marginal branch (right). Both grafts and runoff arteries are widely patent. |
Extra "padding" of tube time was added based on perceived heart rate instability, allowing the reconstruction to adapt to minor heart rate variations. Hsieh et al's adaptive heart rate prediction algorithm was employed to dynamically predict the heart rate for the next cardiac cycle, rather than using a single heart rate for the entire study.
According to the results, 119 of the 121 (98.3%) PGA scans were diagnostic.
"We had two of 21 PGA studies and one of 82 helical CCTA studies that had to be repeated because of artifacts, primarily due to arrhythmias," Earls noted.
Patient doses ranged from 0.75 to 6.67 mSv (mean 2.84 mSv ± 1.3 mSv), representing a mean 83.2% reduction compared to the RGH control group (8.7 to 23.2 mSv, mean 18.4 mSv, p < 0.001).
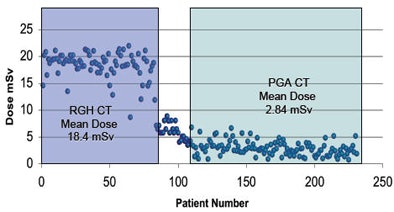 |
| Use of the PGA technique reduced the mean radiation dose by more than 83% compared to standard retrospectively gated coronary CT angiography on the same 64-slice scanner. |
The mean Hounsfield unit density was slightly higher with PGA compared to RGH for the left main, left anterior descending, left circumflex, and right coronary arteries, as well as the aortic root and midleft ventricle. Image noise was consistently lower for the RGH patients, owing to the addition of a noise filter for this group, and the signal-to-noise ratio was consistently higher (p < 0.01).
Image quality was high for both groups, and slightly higher for the PGA patients (mean 4.79 versus 4.51 for the RGH group) across all coronary arteries, a statistically significant difference (p < 0.001; the 95% confidence interval on the image quality increase was 0.20-0.36). Based on image quality scores (two or less considered unevaluable), 1.39% of PGA scores versus 2.11% of RGA scores were deemed nonevaluable. Most patients receiving doses less than 1 mSv were quite thin -- all had BMI scores of 21 or lower.
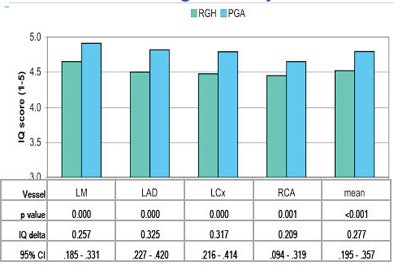 |
| Image quality was slightly higher overall using the PGA technique compared to standard retrospectively gated coronary CT angiography. |
"There was no drop-off in the distal segments with the PGA protocol. In fact the image quality of the PGA studies was better than on the helical exams," Earls stated.
 |
| A 45-year-old male with elevated risk factors and indeterminate exercise stress testing. CTA effective dose using PGA technique was 2.44 mSv. Curved multiplanar reformatted image (left) depicts a stenosis of the inferior branch of the second obtuse marginal coronary artery (OMB2). This was confirmed by conventional coronary angiography (right). |
CCTA performed with the PGA technique is both reliable and robust, reducing by as much as 83% the dose to the patient, he wrote. The significant dose reduction removes one of the most important barriers to widespread clinical use of CCTA, he added.
The method has one limitation worth noting. "Because of the narrow reconstruction windows, neither global nor regional function can be determined with the PGA technique, although expanded acquisition windows with PGA could offer such capability at the cost of a higher dose," Earls wrote. In any case, most patients presenting for CCTA at his institution have already had either an echocardiogram or nuclear myocardial perfusion study to assess function.
"While this is a clear limitation as compared to helical techniques, (it) does not outweigh the added benefits of reduced radiation dose, improved image quality, and adaptive acquisition techniques that reduce or eliminate artifacts from premature contractions," he stated.
In addition to benefiting those with a higher risk of radiation-induced malignancies, patients who might in the future have repeated CCTA studies, such as those with coronary stents, bypass grafts, complex congenital anomalies, or known coronary stenoses, may also benefit because of the lower cumulative dose, he added.
"If additional studies show a potential clinical benefit of serial or periodic evaluation with CCTA, the PGA technique will clearly help minimize their long-term dose," Earls wrote.
By Eric Barnes
AuntMinnie.com staff writer
February 15, 2007
Related Reading
64-slice CT takes on dual-source in cardiac radiation dose, January 26, 2007
Dual-energy CT may assist in coronary plaque identification, January 15, 2007
Inflammatory view: Imaging blind to plaque risk, December 7, 2006
Cardiac CT evolves on multiple fronts, November 15, 2006
Dual-source imaging promises better CT scanning, June 15, 2006
Copyright © 2007 AuntMinnie.com