Musculoskeletal imaging experts may love to chew on the advantages of one imaging modality over another for assessing orthopedic hardware, but the clinicians ordering up these exams are not going to have the same enthusiasm about a rollicking MRI versus CT debate.
"These (orthopedic hardware) patients have special problems that we're trying to solve for the clinicians," explained Dr. Kenneth Buckwalter. "I don't think the clinicians care which (modality) we use. They just want to know the answer. We need to bring our best technology to the table to help them solve the problems."
In a talk at the 2007 Orthopedic Imaging at Pebble Beach conference in Pebble Beach, CA, Buckwalter, who is the clinical director of Indiana Radiology Partners in Indianapolis, discussed ways that imaging experts can optimize their scan technique in the presence of hardware.
Goals
Regardless of the modality used, imaging exams should focus on fracture follow-up, assess prosthetic alignment, and check for fusion or bony bridging, as Buckwalter said he preferred to call it.
"When we are talking about whether or not there is bone crossing a fracture site, we try to guesstimate how much bony bridging there is. We don't use the terms no-union, malunion, or delayed union, which should be avoided on reports," stated Buckwalter, who is also the vice chair of the clinical division for the department of radiology at Indianapolis-based Indiana University.
In fact, Buckwalter stressed that it was best to avoid "red flag" phrases. "We want to exclude potentially inflammatory phrases in our reports. We want to avoid phrases like nonunion or malunion because those are red flags. We want to avoid anything that could be used against an orthopedic surgeon."
 |
| MR scans of normal knee prosthesis. Above, coronal image (TSE: TR 3970, TE 54). Below, sagittal image (TSE: TR 4760, TE 54). All images courtesy of Dr. Kenneth Buckwalter. |
 |
"Certainly, those guys are referring patients to you and we don't want to throw a monkey wrench in, in the event there is a malpractice suit. It's important to keep that in mind when you are dictating examinations," he added.
In terms of prosthetic alignment, Buckwalter described catastrophic failure as "dramatic" and easily seen on imaging. Less obvious are component and screw placement, soft-tissue impingement (relative to hardware placement), and septic and aseptic loosening, especially in patients who develop a reaction to the polyethylene liner.
"Another goal is periprosthetic bone imaging," he said. "Here is an area where we've been able to help out our surgical colleagues tremendenously by defining how much periprosthetic bone is available to them when they do a revision arthroplasty."
Hardware
While it may seem reasonable that orthopedic surgeons won't be interested in the nitty-gritty of the imaging exams, don't be surprised if they also don't have a lot to say about the types of hardware that they placed in their patients.
"When you have patients with metal hardware who come to you for imaging, you won't know what the hardware is, and it's not practical to find the surgeon and ask them because they won't remember," Buckwalter said.
Most metal hardware can be categorized as cobalt-chrome, iron, titanium, and oxidized zirconium (Oxinium). Cobalt-chrome is found in the older generation of hip prostheses. Iron is often used for plates and screws, as is stainless steel. Titanium is commonly used for fixation plates and screws.
When it comes time to figuring out the type of hardware, Buckwalter recommended relying on the scout view. If the metal is dense, it will appear white on scout view while titanium will be gray.
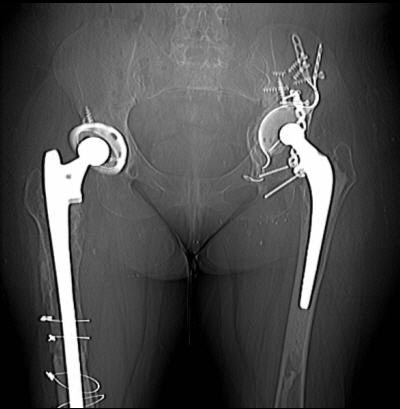 |
| CT scan of a 58-year-old woman with catastrophic hip failure. |
With regard to artifacts, cobalt-chrome is associated with significant artifacts, as are iron and iron alloys. As a less dense metal, artifacts on titanium are not a big problem. Oxidized zirconium should pose even less of a problem because it is lighter metal, Buckwalter said.
"The prostheses are changing every year," Buckwalter pointed out. "One of the things that is very hot now is ceramic- and metal-bearing prostheses, so we are going to see different kinds of delayed problems as the surgeons migrate away from polyethylene to other kinds of bearing elements in the prostheses. It's going to be an interesting time, and we are still going to need to have techniques to image around prostheses."
CT
Nonimaging specialists are often under the mistaken impression that the presence of metals rules out the use of CT. But quite often the hardware is located above or below the joint line, enabling CT to demonstrate pathology in the joint space, Buckwalter said.
In addition, CT is best for direct visualization of bone and hardware, he continued, adding that CT gives a better idea of what metal components are involved and what their shapes are. Knowing more about the hardware itself can offer valuable clues on the mode of failure. While CT has very high spatial resolution, the soft-tissue visualization is fair to poor around metal.
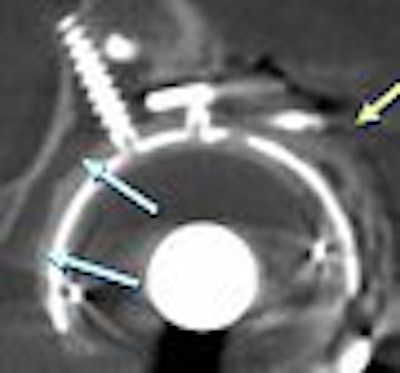
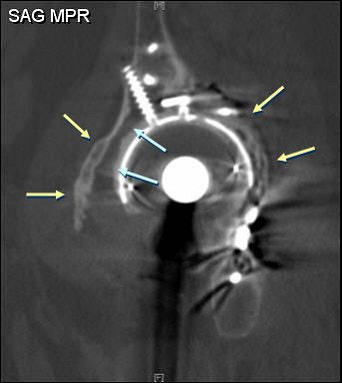
 |
| A 61-year-old woman with bilateral hip prostheses who was referred before surgery for evaluation of remaining "bone stock" surrounding cetabular hardware. Multislice CT was performed with thin slices (2.5-mm slice width, 1.4-mm reconstruction interval), high kilovoltage (140 kVp), and high tube current (750 mAs). Coronal reformatted image shows sparse amount of bone surrounding acetabular components (solid arrows). Wear of plastic joint liner of right hip (open arrow) is shown. Optimal scanning technique minimized metal artifacts. Buckwalter KA, Rydberg J, Kopecky KK, Crow K, Edward L, Yang EL, "Musculoskeletal Imaging with Multislice CT" (American Journal of Roentgenology, 2001; 176:979-986). |
Hardware-related artifacts are at their worst closest to the densest metal. "Artifacts are always in the direction of greatest metal bulk," Buckwalter advised. "So if you know that there is a lateral side plate, there's a high probability that you are going to be successful medial to the plate. The streaking artifact is going to be in the anteroposterior axis of the plate."
Buckwalter suggested the following CT protocol for hardware:
 |
| CT technique ('big metal') |
 |
|
 |
If a region of interest does not contain metal, there is the option of repositioning the limb that contains the hardware outside of the scanner. For example, a patient with a knee prosthesis may complain of pain in the opposite knee, which did not undergo surgical replacement. In that instance, "the contralateral knee can be elevated and bent to prevent artifacts from propagating across to the knee in question," Buckwalter wrote in the course syllabus.
MRI
MRI has moderate spatial resolution, but, of course, excels at visualizing soft tissues. MRI offers indirect visualization of the cortical bone and hardware, Buckwalter stated. "Metal-friendly" MR sequences are fast spin echo and fast STIR. On the other hand, gradient echo, fat saturation, and spin echo are of little use for hardware-centered MR.
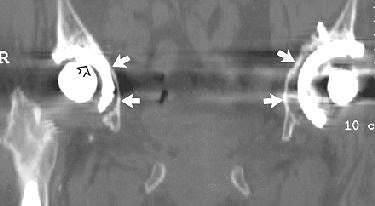
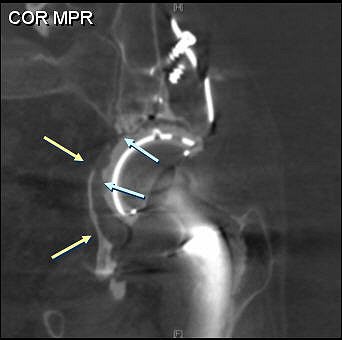 |
| MR scans of a 58-year-old woman with catastrophic hip failure. |
 |
On MRI, artifacts occur mainly in the frequency-encoded access of the image, he said. "If you can't see what you want to see in one direction, you can ask the technologist to do another acquisition, swamping frequency and phase," he advised.
Buckwalter suggested the following MR protocol:
 |
| MRI technique |
 |
|
 |
While MR vendors may not mention musculoskeletal imaging in their sales pitch for bigger, better magnets, hardware imaging provides an opportunity to use what Buckwalter called "sexed-out" machines.
"Most of the time, when those (MR) sales people come by, they want you to buy the highest gradient platform so you can do cardiac imaging, diffusion tensor, and other really sexy stuff. Orthopedic imaging is also improved when you have access to better gradients. At least one of your magnets in your stable of magnets should be a totally sexed-out machine and that's the one you want to do your metal imaging on," he said.
By Shalmali Pal
AuntMinnie.com staff writer
May 4, 2007
Related Reading
Scout view: Imaging helps football prospects sack injuries at NFL Combine, February 20, 2007
The ABCs of MRI for hip disorders, February 2, 2007
From tears to TKA: The ins and outs of knee MRI, September 5, 2006
Copyright © 2007 AuntMinnie.com