LOS ANGELES - As radiation oncologists continue to push the envelope with dose escalation, imaging guidance becomes an indispensable tool for treatment planning, assessing response relationships, and, ultimately, reducing morbidity.
To that end, three presentations at this week's American Society for Therapeutic Radiology and Oncology (ASTRO) meeting looked at the role CT plays in targeting and planning. In the first paper, radiation oncologists at Houston's M. D. Anderson Cancer Center attempted to standardize dosing methods with 4D CT measurements of lung volume.
In a second study, investigators from William Beaumont Hospital in Royal Oak, MI, wanted to detect potential target dosage in breast cancer patients undergoing external beam accelerated partial breast irradiation (EB-APBI). In another presentation, German investigators evaluated the reliability of bony anatomy in image-guided stereotactic radiotherapy of brain metastases.
4D CT
Respiratory motion has always been a challenge in thoracic radiotherapy, said Dr. Yixu Kang in her ASTRO talk. She and her colleagues conducted a retrospective study in 40 stage III/IV non-small cell lung cancer (NSCLC) patients who underwent 4D CT scans and fast free-breathing helical CT (FBCT) scans. All lungs were contoured in the FBCT and 4D CT datasets at the end of expiration (EXP) and end of inspiration (INSP).
"A special time-averaged CT was created by averaging CT numbers in the same spatial voxel over all reconstructed phases of the 4D CT. This represents the time-averaged lung density (AVE). We compared various lung volumes using EXP CT as the reference volume," the group wrote in its ASTRO abstract.
The researchers compared the dose variations and dose-volume effects for lung tissue using the same treatment plan in EXP, INSP, AVE, and FBCT datasets in 15 of 40 patients. They then compared the percentages of lung exposed to a range of radiation, from 5 Gy to 50 Gy (V5, V20, V50).
Finally, they performed an alternative dose-volume histogram (DVH) calculation using the same dose distribution on a single CT, but normalized to the lung volume on a different CT dataset.
According to the results, the total lung volumes were 13.9% higher on INSP CT than those defined on EXP CT sets. Lung masses defined on INSP CT sets were 4.6% higher on INSP CT versus EXP CT. The average INSP lung density was 8.0% lower than the EXP lung density. On average, the free-breathing total lung volume was 6.3% higher and the AVE lung volume was 8.8% higher than the lung volume defined on EXP CT.
The authors said they found a "strong volume effect" for the dose-volume relationships using different lung volume definitions. The total lung dose was higher in INSP CT than in EXP CT across the board as the dose escalated:
- V5: 3.3% higher
- V20: 2.4% higher
- V50: 2.0% higher
"We found that using a simple volume scaling factor can effectively convert the DVH results from one CT lung volume into another," the group wrote. "The INSP and EXP V5, V20, and V50 values can be predicted more accurately from dose distributions calculated on AVE CT than those calculated on FBCT."
"We believe standardized reporting can lead to better interpretation of existing data and more accurate reporting of future studies," said co-author Dr. M. Kara Bucci in a written statement. "This will lead to improved risk assessment in planning individualized patient care."
Planning APBI
For the William Beaumont-based research, 16 patients with early-stage disease had postlumpectomy EB-APBI. The clinical target volume to planning target volume (CTV-to-PTV) margin was 10 mm. The patients had conebeam CT (CBCT) scans prior to each fraction (10 scans per patient) and daily helical CT scans (five per patient).
"CBCT images obtained prior to each fraction were automatically registered to the planning CT to determine translational/rotational setup errors," the authors explained. In addition, the helical CT scans were imported into the planning system in treatment positions specified by CBCT scans. The cavity was contoured and dose per fraction was calculated in the helical CT scans. An in-house image intensity-based deformable registration program was used to register the helical CT scans to the planning CT scans to generate cumulative dose.
The treatment schedule was 38.5 Gy in 10 fractions twice a day, over five days. The following parameters were used to compare the cumulative reconstruction and initial plan for each patient: PTV_EVAL V90, ipsilateral breast V50 and V100, lung V30, heart V5, and MaxDose. These dose constraints were based on a National Surgical Adjuvant Breast and Bowel Project trial protocol (NSABP B39).
According to the results, the mean setup error magnitude based on CBCT registration was 9 ± 5 mm. The mean percent change in cavity volume between the planning CT and treatment day one was -32 ± 35% over a median of 23 days with 88% of the patients showing volume decrease.
"Between the first and last treatment day (relative to the planning CT volume), the mean percent change in cavity volume was 1 ± 21%, with seven of 16 patients showing increasing cavity volume. DVH analysis showed one patient with a decrease in CTV V90 of 8%. All other patients demonstrated adequate target coverage with reduction in CTV V90 ≤ 1%," the authors wrote.
Other results included PTV_EVAL V90 coming in 3% less than planned. For the ipsilateral breast, four patients had a maximum 1% increase in V50 and three patients had a maximum 9% increase in V100. Four patients had a maximum 3% increase in ipsilateral lung V30. One patient had a maximum 1% increase in heart V5. Finally, four patients had an increased in MaxDose (maximum increase of 89 cGy).
Based on CT planning, the CTV-to-PTV margin of 10 mm was sufficient in about 93% of the patients, the authors concluded. Expanding the PTV to 14 mm would provide a 97% confidence level of CTV coverage, but this would require online imaging, they stated.
Bony anatomy
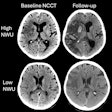
In the third study, Dr. Michael Flentje and colleagues from the University of Würzburg looked at 20 brain metastases in 18 patients who were treated with single fraction or hypofractionated image-guided stereotactic radiosurgery. Patients were immobilized in either stereotactic Scotch-cast (SC) masks or thermoplastic (TP) head masks.
CBCT images were acquired prior to treatment (Synergy S, Elekta, Norcoss, GA) and patient setup was evaluated by automatic image registration with the planning CT (XVI SW, Elekta). The bony anatomy of the skull was the basis for this image registration. Finally, a conventional contrast-enhanced CT study was acquired for all patients using an in-room scanner (Tomoscan M, Philips Medical Systems, Andover, MA).
"Patient setup was evaluated based on the position of the brain metastases," the group wrote. "Results of bone match and soft-tissue match for verification of patient setup were compared."
According to the results, the median time interval between planning and treatment was eight days. Based on automatic bone registration of CBCT and planning CT, the 3D positioning error was 3 mm ± 1.7 mm for patients immobilized in SC masks. For those in TP masks, the 3D positioning error was 4.6 mm ± 2.1 mm. Tumor size was not significantly different between treatment and planning.
The 3D setup error was 4 mm ± 2.1 mm based on the bony anatomy and 3.5 mm ± 2.2 mm based on the lesion itself. The distance between the iscocenter based on bone match and soft-tissue registration was 1.7 mm ± 0.7 mm. The authors reported a highly significant correlation between automatic bone match and soft-tissue registration.
Even with a one-week interval, "the bony anatomy of the skull proved an excellent surrogate for the target position on image-guided stereotactic radiosurgery," the group concluded. The researchers noted that 3D image registration for verifying patient setup with stereotatic masks was less reproducible than with 2D registration, which emphasized the importance of CT guidance for stereotactic radiotherapy.
By Shalmali Pal
AuntMinnie.com staff writer
October 30, 2007
Related Reading
PET/CT is powerful for radiation therapy planning, May 4, 2006
Cosmetic results good, toxicity mild with accelerated partial-breast irradiation, March 20, 2006
Radiotherapy for perineural spread of skin cancer to brain may extend survival, June 9, 2005
Copyright © 2007 AuntMinnie.com