One of the many ways in which radiology represents both art and science is in the assessment of solitary pulmonary nodules (SPNs), which must either be followed over time to evaluate growth, or resected or biopsied -- with the latter two options injecting cost and risk into the equation.
Size, morphology, location, and of course the radiologist's studied impressions all play important roles in the decision to follow or biopsy. And while nodule growth over time, especially rapid growth, increases the likelihood of malignancy, growth or lack thereof offers no guarantees.
Even the best currently available technology for measuring nodules noninvasively, automated CT volumetric measurements, is imprecise. Radiologists following up CT-detected nodules must also distinguish between incremental changes in size and other factors, such as interscan variability, that influence volume measurements.
The question has important clinical implications due to greatly increased surveillance of SPNs detected at chest CT scans acquired for various reasons including lung cancer screening. This article examines recent reports on the subject.
First, in a new study appearing in the October issue of Radiology, Dutch researchers prospectively evaluated the accuracy of semiautomated lung volume measurements in 20 patients by scanning them twice at low doses to investigate the influence of nodule size, segmentation algorithm, and inspiration levels. Reported volumes varied by more than 20%. Another group from the Netherlands examined the relation of shape and density to malignancy.
Second, in a presentation at the 2007 International Symposium on Multidetector-Row CT in San Francisco, one of the authors of the aforementioned Radiology study, Dr. Mathis Prokop, discussed the evidence-based decision to follow up or resect SPNs based on volume doubling time, and accounting for the measurement variability.
Variable nodule size
"Three-dimensional measurements have been shown to be more accurate and are therefore more often applied in lung cancer screening trials," wrote Dr. Hester Gietema, Ph.D., and colleagues. "The purpose of our study was to prospectively assess the precision of semiautomated volume measurements of pulmonary nodules at low-dose multidetector-row CT, and to investigate the influence of nodule size, segmentation algorithm, and inspiration level" (Radiology, October 8, 2007).
The study examined 20 patients (15 men and five women, ages 40-84) who were referred for chest CT for known lung metastases for two additional noncontrast low-dose chest scans.
The scans were acquired on a 16-slice CT scanner (Mx8000 IDT, Philips Medical Systems, Andover, MA) at 30 mAs and 120-140 kVp, using 16 x 0.75-mm collimation. Images were reviewed on a Leonardo workstation (Siemens Medical Solutions, Erlangen, Germany), and semiautomated volume measurements were performed with Siemens LungCare software.
Between the two scans, patients got off the table to simulate returning for a follow-up scan, the authors wrote. Only noncalcified solid pulmonary nodules between 15 and 500 mm3 not adjacent to a vessel or pleura were measured, and the group recorded whether each nodule was spherical or nonspherical in shape.
"We visually determined the precision of the measurement software by assessing whether the nodule was completely segmented," wrote Gietema, along with Dr. Cornelia Schaefer-Prokop, Ph.D.; Dr. Mathias Prokop; and colleagues at the University Medical Center Utrecht and the Academic Medical Center, Amsterdam, both in the Netherlands.
"Nodules were categorized into two groups (A and B) on the basis of whether the yellow overlay completely matched the nodule, or whether visual assessment determined a mismatch (group B)," they explained.
The software evaluated 218 eligible nodules (volume range 16.4-472.7 mm3) including 106 spherical (having a constant radius) and 112 lobular nodules (having an irregular radius but smooth outer margins).
According to the results, the 95% confidence interval for the difference in measured volumes was -21%, 23.8% (mean difference 1.3%). The segmentation accuracy was highly dependent on nodule shape (p < 0.001), and there was also a weak relation to the inspiration level for completely segmented nodules (r = -0.20; p < 0.47). Mean nodule volume did not vary between the scans (p = 0.15 and p = 0.81 for spherical and nonspherical nodules, respectively).
"Results of previous studies have shown that the applied software is very accurate for small spherical nodules, but our results suggest that the precision may vary substantially with nodule morphology," the authors wrote. "While the precision was extremely high for spherical solid nodules, the precision decreased for nonspherical or irregularly shaped nodules."
"This is especially noteworthy considering the fact that many nodules detected in a lung cancer screening setting do not have perfectly spherical shapes with smooth margins," they reported. "Thus, assessment of the volume of such nodules with the semiautomated software we tested might be prone to considerable variation."
The accuracy of the software was highly dependent on nodule morphology, and results were less reproducible for nonspherical compared to spherical nodules, though the extent of variability decreased with increasing nodule size and higher inspiration levels, the researchers found. The use of a single software algorithm was cited as the single most important limitation of the study.
"Taking the reported variation into account, the threshold for calling an increased measured volume of a lung nodule a real volume increase with 95% confidence lies at a 30% increase for an irregularly shaped lesion," they concluded. "For spherical nodules, this threshold can be lowered to 15%."
On the subject of shape, a new study by Xu and colleagues at the University Medical Center Groningen in the Netherlands examined the relationship of shape and density to malignancy in 469 indeterminate or potentially malignant solid pulmonary nodules (> 50 mm3). Results were presented as likelihood ratios (LR) with 95% confidence intervals.
In a multivariate analysis, lobulated nodules had an LR of 11 compared to smooth nodules, Xu et al reported. Spiculated nodules had an LR of 7 compared to smooth, irregular nodules had an LR of 6 compared to round and polygonal. Volume had an LR of 3 (European Journal of Radiology, October 5, 2007).
"In solid noncalcified nodules larger than 50 mm3, size and to a lesser extent a lobulated or spiculated margin and irregular shape increased the likelihood that a nodule was malignant," Xu and colleagues wrote. "Nodule density had no discriminative power."
Assessing doubling time as a factor in malignancy
The concept of significant growth is interesting because "it says something has grown but doesn't necessarily say that a nodule is benign or malignant," said Dr. Mathias Prokop in his talk at the 2007 International Symposium on Multidetector-Row CT. "The basic problem is that small nodules less than 10 mm occur quite frequently, especially in some American populations," and their small size makes them difficult to biopsy, he said.
"The important factor is the speed of growth, as measured by volume doubling time, a complex formula (VDT = Δt x lg2 / lg[V2/V1]) that measures the interval between time point one and time point two," Prokop said. Based on the concept of exponential growth, VDT represents the time it takes for a nodule to double (i.e., 100% increase in volume).
Compared to volume, diameter measurements are a poor way to assess growth, Prokop said. A nodule that has grown in diameter from 8 mm to 9.6 mm shows a 10% change in diameter, but a 64% increase in volume, which is much easier to measure and evaluate.
To date, several studies have documented mean differences in volumetrically measured VDT between benign and malignant SPN, notably Dr. David Yankelvitz et al (Radiology, October 2000, Vol. 217:1, pp. 251-256).
The researchers from New York-Presbyterian Hospital and Weill Cornell Medical Center in New York City tested the measurement results in synthetic nodule phantoms, and in a group of 13 patients with biopsy-proven results. They found median volume doubling times of 177 days for malignant nodules and 396 days for benign nodules in 13 patients, Prokop said.
Last year Dr. Marie-Pierre Ravel and colleagues from L'Assistance Publique - Hôpitaux de Paris found similar results with 52 benign and 11 malignant noncalcified nodules (American Journal of Roentgenology, July 2006, Vol. 187:1, pp. 135-142).
Ravel et al found that the mean VDT for malignant nodules was 117 days, versus 947 days for benign nodules. Using a VDT cutoff value of 500 days, sensitivity and specificity for detecting malignancies was 91% and 90%, respectively, with negative and positive predictive values of 98% and 67%, respectively, Prokop noted.
In another new study by Xu et al from Groningen, data from the NELSON Dutch Lung Cancer Screening Trial were used to evaluate VDT in purely intraparenchymal nodules 50-500 mm3 (≈ 4.5-10 mm). In results submitted for publication, 75% of nodules with doubling times less than 400 days were malignant, compared to 9% of those with VDT of 400-600 days, and 0% of nodules with VDT longer than 600 days, Prokop said.
Thus, a fast VDT really does appear to be predictive of malignancy, he said. "If you use software, usually 25% growth is a relatively decent cutoff point to say, 'OK, this nodule has really grown and it's not a measurement error.' "
But finding the right VDT cutoff point for determining the nodule's malignancy or benignity is a tricky proposition, Prokop said. "Depending on this cutoff point, you could either call too many nodules growing, and therefore get too many unnecessary interventions, or you could actually miss growing nodules and cancers -- so it's very important," he said.
For example, if significant growth requires a greater than 25% increase in volume (accounting for measurement error), then all significantly growing nodules detected at less than a four-month follow-up have a VDT less than 400 days and are suspicious for malignancy.
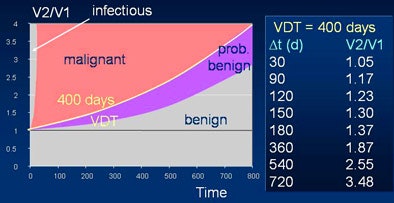 |
| Based on volume doubling time of 400 days, chart shows hypothetical probability of malignancy rising with growth over time (V1 = initial volume, V2 = volume at follow-up). Chart courtesy of Dr. Mathias Prokop. |
But in the same four months, a fast-growing tumor with a VDT of 30 days "would have increased in size by a factor of eight," Prokop said.
A slow-growing nodule followed up in four months may not yet show significant growth, so these nodules need longer follow-up to show significant growth, for example at six months and one year. At both the six- and 12-month follow-ups, VDT has to be calculated to determine likelihood of malignancy, Prokop said.
At 12 months even the slow-growing nodule would have grown by 87%. However, "by that point significant growth doesn't say that this is necessarily a malignancy," Prokop said. "At this point you have to look at VDT to determine what you're going to do with these patients."
Three months appears to be a sensible compromise between too-frequent follow-up and too-late detection, he said. A problem with the concept of VDT is that it relies on a constant exponential growth rate. "Some tumors have a volume doubling time that varies, tumors that arise from benign disease, or faster-growing nodules within a relatively slow-growing tumor," Prokop said.
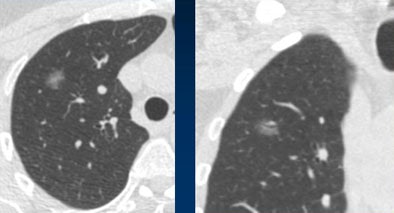 |
| Stable ground glass nodule showed no growth at three months or one year, but grew slightly over three years' time. Histology revealed a bronchoalveolar cell carcinoma. Image courtesy of Dr. Mathias Prokop. |
VDT measurements of perifissural nodule growth are poor indicators of malignancy, he said; perifissural nodules often grow then shrink again. The rule of thumb for malignancy is no continuous growth over six months.
Nodules at high risk of malignancy include growing ground-glass nodules, stable or growing part-solid nodules, and growing solid nodules with a VDT less than 400 days, Prokop said. At a low risk of malignancy are typical perifissural nodules and growing solid nodules with a VDT greater than 600 days.
"Volumetry is essential for the correct estimation of volume doubling times," Prokop concluded. "Diameter measurements are far less reliable, and you always have to check to see if the segmentation is correct. However, VDT is only important for solid nodules, and it implies exponential growth, which is unfortunately not always true."
By Eric Barnes
AuntMinnie.com staff writer
November 5, 2007
Related Reading
Radiologists no match for nodule measurement software, August 31, 2007
SUV readings vary on different PET systems, study finds, July 25, 2007
Low-dose CT practical for lung cancer screening, April 30, 2007
Part I: Automated CT lung nodule assessment advances, April 17, 2006
Copyright © 2007 AuntMinnie.com




















