Used as a preoperative planning tool, multidetector-row CT angiography reduces the number of aborted pancreatic resections, according to new research from Beth Israel Deaconess Medical Center in Boston. The retrospective study found that the addition of contrast significantly improved the detection of vascular invasion that prevented curative resection.
A high surgical complication rate of 2.5% to 5% makes it critical to identify patients who would most benefit from pancreatic laparotomy and exclude those who would not, wrote Dr. Giulia Zamboni, Dr. Jonathan Kruksal, Dr. Charles Vollmer, and colleagues in the December issue of Radiology.
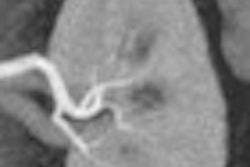
"Classic criteria for defining unresectability at helical computed tomography include extrapancreatic invasion of adjacent tissues and organs other than the duodenum, stenosis, or semicircular encasement of any major peripancreatic vessel," they wrote, noting that CT is not accurate in predicting nodal involvement, and CT depiction of peripancreatic nodes "should not prevent an attempt at curative resection in patients presumed to have pancreatic carcinoma that is otherwise resectable" (Radiology, December 2007, Vol. 245:3, pp. 770-778).
Predictive values for CT are high for determining unresectability, between 89% and 100%, they noted. However MDCT's predictive values for unresectability are far lower, ranging between 45% and 79%, according to the authors. And compared to CT, CTA with 3D reconstruction offers additional information and improves staging for resectability, predicting vascular resectability at 96% for CTA versus 70% for CT alone (p = 0.021) in a 1997 study led by Beth Israel's Dr. Vassilios Raptopoulos, who participated in the current research.
In this study, Zamboni and his colleagues aimed to "retrospectively assess the sensitivity and specificity of MDCTA in the preoperative evaluation of pancreatic adenocarcinoma, by using surgical findings as the reference standard," they wrote.
To that end, the group reviewed CT reports, surgical notes, and pathology reports from 114 patients with pancreatic or distal cholangiocarcinoma who underwent both MDCTA and surgery at Beth Israel between 2003 and 2006. In cases where findings were discordant, experienced readers examined the images for lesion resectability.
Images were acquired on a variety of MDCT scanners: 4-, 8-, 16- and 64-slice models in 54, 19, 25, and 16 patients, respectively. Collimation was set at 1.25 mm for the 4- and 8-slice scanners, and 0.5 mm and 0.625 mm for 16-slice and 64-slice CT. (Aquilion 16, Aquilion 64, Toshiba America Medical Systems, Tustin, CA; LightSpeed Plus, LightSpeed Ultra, LightSpeed Pro16, LightSpeed VCT, GE Healthcare, Chalfont St. Giles, U.K.)
"Patients underwent scanning with similar techniques and protocols, including unenhanced, late arterial/early portal venous and venous acquisitions, timed with a bolus-tracking technique." A 150-HU threshold was used to determine scan timing, Zamboni and colleagues wrote.
Transverse images, multiplanar reconstructions, coronal and sagittal reformations, and thick-slab oblique scans "along the planes of the great vessels were viewed on PACS for the initial interpretation," they explained. Criteria for unresectability included distant disease, invasion of adjacent organs (except the duodenum) and major vascular invasion.
The results showed that 88/114 patients (46 women, 42 men, mean age 67 years) had resectable lesions according to CTA criteria, constituting group A. The resection was aborted in 10 patients (11%). Group B consisted of 16 women and 10 men, mean age 62, whose lesions were confirmed as unresectable.
The initial clinical interpretation of the CTA scans yielded 100% sensitivity for the detection of resectability, 72% specificity, 89% positive predictive value, and 100% negative predictive value -- and the results did not appear to vary according to scanner type. Following blinded retrospective evaluation by experienced readers, specificity rose to 94% and positive predictive value to 98%, while sensitivity and negative predictive values did not change.
In a specialized diagnostic setting using thin collimation, a high-contrast injection rate and multiphasic imaging, preoperative MDCTA is an effective tool that reduces the number of aborted pancreatic resections, they concluded.
Still, "Only 60% to 91% of the tumors judged resectable at CT are truly resectable, whereas the others manifest local tumor invasion, lymph node metastases, or small hepatic or peritoneal metastases," Zamboni et al wrote. "This finding was confirmed by the results in our series, in which 89% (78 of 88) of the tumors deemed resectable at CT angiography were truly resectable."
As for study limitations, the institution specializes in pancreatic disease, the team wrote, and therefore occasionally attempts a "heroic" surgery effort even when the criteria indicate unresectability, or undertakes surgery in order to confirm the diagnosis. In addition, the series was small in order to make the cohort as homogeneous as possible, and therefore limited in its statistical power.
"Strict adherence to technical scanning and image-processing protocols and close attention to the CT signs at the time of interpretation are imperative," they wrote.
By Eric Barnes
AuntMinnie.com staff writer
December 25, 2007
Related Reading
Link between obesity and cancer stressed in report, November 1, 2007
MDCT's 'virtual Whipple' offers practice run before complex surgery August 16, 2007
High contrast flow rate best for pancreas CT, November 8, 2006
Elderly need less contrast for pancreatobiliary imaging, August 2, 2006
CT features diagnose autoimmune pancreatitis, February 2, 2006
Copyright © 2007 AuntMinnie.com