
The Fort Defiance Hospital and the Tuba City Medical Center flank the southern and western ends of a vast Native American homeland known as Navajo Nation. Straddling the states of Arizona, Colorado, and Utah, the semiautonomous region is home to more than 175,000 Navajo. Pride and an enduring sense of tribal identity have kept culture and social cohesiveness intact through massive changes the last century has brought.
But access to healthcare remains spotty in the region, a patchwork of reservations and federal lands encompassing 26,000 square miles. Transportation to the two main medical centers is difficult for some patients, and telephones are scarce.
Recruited by the University of Arizona to establish a remote virtual colonoscopy service for the poor and largely underserved rural population, Tucson radiologist Dr. Arnold Friedman might have been forgiven for having, well, reservations. But he found that determination, patience, and a dedicated onsite staff were important allies in delivering state-of-the-art colon cancer screening services to the hardscrabble homeland.
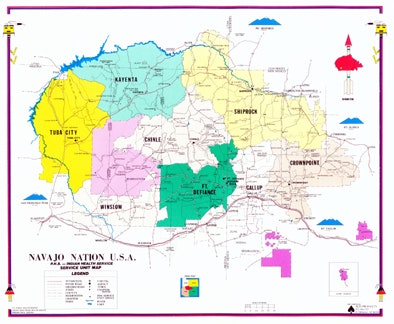 |
| The Navajo Nation encompasses 26,000 square miles in the states of Arizona, Colorado, and Utah. Map of the Navajo Nation courtesy of Indian Health Service. |
People there "have limited access to optical colonoscopy and other forms of outpatient cancer screening," said Friedman, a professor of diagnostic radiology at the University of Arizona, Tucson, at the 2008 International Symposium on Virtual Colonoscopy in Boston. "At the University of Arizona we were already interpreting a large percentage of their imaging studies via teleradiology, and our goal is to expand the service to include CTC [CT colonography or virtual colonoscopy] for colon cancer screening. The question we want to answer is can adequate exams be obtained with remote supervision after a brief onsite instruction."
Fort Defiance Hospital has a 24-hour level II emergency department that operates with 56 beds and more than 235,000 outpatient visits a year, Friedman said. There are no gastroenterologists, but there are four surgeon-endoscopists who can intervene when virtual colonoscopy results are positive. Farther west, Tuba City handles some 20,000 emergency room visits a year and 211,000 outpatient visits. It has 65 beds, 57 physicians, and again no gastroenterologists, but three surgeon-endoscopists.
Friedman made the seven-hour drive to Fort Defiance and gave technologists from both medical centers a lengthy PowerPoint presentation on virtual colonoscopy, finally performing the exam on a volunteer. Since then, more than 100 exams have been performed, Friedman said, all scanned solely by radiologic technologists and interpreted remotely by University of Arizona radiologists.
The bowel preparation consists of a magnesium carbonate and potassium citrate powder (LoSo Prep, Bracco Diagnostics, Princeton, NJ) with a (Tagitol, Bracco Diagnostics) barium suspension ingested with meals for fecal tagging. The health center pharmacies mail the supplies to patients to ingest at home beginning two days before the scan. Delivery "works pretty well," Friedman said.
Automated CO2 insufflation of the colon is performed before the CT scan using a ProtoCO2l pump (Bracco Diagnostics) and scout images are acquired to ensure the adequacy of insufflation. The technologists acquire routine supine and prone scans at 120 kVp and 50 mAs (supine) and 25 mAs (prone). Volumes (1 mm x 1 mm) are then transmitted to the university's local teleradiology server and uploaded to a CTC workstation.
"It took roughly 10 to 20 minutes to transmit images to our teleradiology server, then another five minutes to upload from the server to the CTC workstation," Friedman said. He and his colleagues Caroline Kilian, Dr. David Downing, Dr. Joachim Chino, and Dr. Peter Lance have interpreted about 100 exams since May, Friedman said.
The first 25 patients included 11 women and 14 men (mean age, 58.7 years; range, 37-88). The indications were screening (n = 22), diverticulitis (n = 2), and one patient with iron deficiency anemia.
"I graded exam quality and evaluated residual stool on a five-point scale," Friedman said. "Any difficulties were noted, I called the techs with other problems, and created C-RADS categories from the clinical reports," he said.
Technical problems in those first 25 patients included a case of vaginal insufflation one day when the regular technologist was absent. In another case, the splenic flexure was cut off on the prone images. And there have been a few virtual colonoscopy exams that might have been unnecessary, including a 37-year-old man with suspected diverticulitis, and two very elderly patients (an 88-year-old man and an 84-year-old woman) who probably shouldn't have been screened for colorectal cancer, Friedman said.
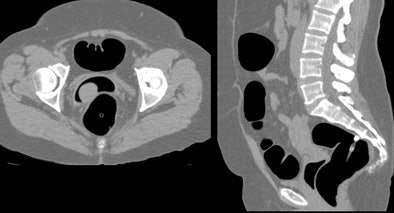 |
| Occasional errors occurred with the use of unsupervised technologists to perform virtual colonoscopy scans. In one instance, a substitute technologist who had not been trained in virtual colonoscopy performed a vaginal intubation and insufflation in error. After the tube was removed and reinserted in the rectum, the colon was insufflated successfully and the patient scanned without incident. Image courtesy of Dr. Arnold Friedman. |
Among the first 25 exams, there were four (16%) C-RADS C0 cases, that is, inadequate exams that could not be interpreted, Friedman said. "Of these four, two occurred on a day when the regular tech called in sick, so those two were done by a tech with no training," he said. One patient didn't take the prep at all. So really we had only one uncorrectable [C-RADS] C0, which isn't too bad." (For this story, Friedman also provided AuntMinnie.com with an updated abstract that included an analysis of 86 of the first 100 patients.)
One patient was unable to retain the CO2 gas. "I told them to put in a large rectal tube and a large [retention] balloon to tape the cheeks," Friedman said. And we got a perfectly adequate scan."
 |
| One patient was unable to retain the CO2 gas during insufflation. The problem was solved with the addition of a large rectal catheter and a retention balloon, and by taping the buttocks together. Image courtesy of Dr. Arnold Friedman. |
In three of 86 patients, the readers observed a partial rectal cutoff in the prone image set only. There were seven cases with respiratory motion artifact, none of which seriously interfered with interpretability. In one patient dense iodinated contrast in the stomach caused an image artifact, the researchers reported in their abstract.
"Each incident was discussed by phone with the responsible CT technologist," Friedman said.
The assessment of residual stool (1-5 scale, with 5 meaning almost no residual stool) revealed 43 patients at 5/5, 20 patients at 4/5, 18 patients at 3/5, one patient at 2/5, and three patients at 1/5 (including the patient who was scanned without taking the prep).
The assessment of residual fluid (1-5 scale, with 5 meaning almost no intraluminal fluid) revealed 37 patients at 5/5, 27 patients at 4/5, 16 patients at 3/5, two patients at 2/5, and three patients at 1/5. One patient failed.
The assessment of distension adequacy (1-5 scale, 5 meaning all segments were well distended in both positions) revealed 36 patients at 5/5, 11 patients at 4/5, 13 patients at 3/5, 17 patients at 2/5, eight patients at 1/5, and the same patient failed.
Additional technical problems included a splenic flexure cutoff on prone images (n = 2, area seen well supine on both) and excess photopenia in an obese patient, which hindered interpretation (n = 2).
Sixty-seven of 86 patients had normal findings, two had subcentimeter polyps (C-RADS C2), and seven patients had polyps 1 cm and larger (C-RADS C3), including one false positive, one true positive, one failed exam, and several unconfirmed findings. Assuming half of the C2 patients with small polyps chose optical colonoscopy over surveillance, the referral rate to conventional colonoscopy was 9%, Friedman said.
Three C-RADS E3 extracolonic findings of potential clinical importance included an ovarian mass, a right lower lobe lung nodule, and a probable pedunculated fibroid. Clinically significant extracolonic findings (C-RADS E4) included (one each) a metastatic renal cell carcinoma, cirrhosis, bilateral pleural effusions, porcelain gallbladder, a possible lung carcinoma, and a huge fibroid uterus compressing the sigmoid colon.
"Virtual colonoscopy can be introduced with minimal effort to rural underserved communities, adequately performed locally, and then interpreted remotely by an expert," Friedman concluded. "You have to explain the indications repeatedly, and establish an upper age limit. Techniques such as the avoidance of vaginal insufflation, colon cutoff, and motion artifacts should be explained to novice technicians."
After 100 exams "the results are still pretty good," Friedman said. "The referral rate for optical colonoscopy is about 9%, which correlates with published figures."
Dr. Michael Zalis from Massachusetts General Hospital and Harvard Medical School in Boston congratulated Friedman on his success. "Having worked in Fort Defiance as a medical student many years ago, I want to commend you for all of the effort it takes," Zalis said. "I know what a rural setting this is and what little access the Navajo population around there has to the medical system."
Another attendee said that "one of the great benefits of CT is that it can operate in that kind of a setting. If you have a scanner in a rural setting, a lot of people who don't have access to colon screening can come and get their exam, and the small percentage that have significant lesions can be appropriately evaluated, so great work."
The issue of same-day colonoscopy is complicated by the time needed to transmit the virtual colonoscopy images to Tucson and read them before the patient goes home, Friedman said in response to a question after his talk. But a half-hour delay does not present an insurmountable barrier to same-day exams, he said.
By Eric Barnes
AuntMinnie.com staff writer
November 18, 2008
Related Reading
Teleradiology paves way for remote medicine, October 16, 2008
VC training course expands with teleradiology, July 21, 2008
Teledermatology project moves toward DICOM standards, July 15, 2008
Asians least likely to receive CRC screening in U.S., June 25, 2008
Online games urge Native American women to b-i-n-go for mammograms, August 30, 2005
Copyright © 2008 AuntMinnie.com




















