Lung cancer staging will undergo important changes following publication this year of the new edition of the tumor, node, and metastasis (TNM) classifications for lung cancer. Although much will improve compared to the current guidelines, thanks in large part to better data, important limitations will remain.
The new criteria is the culmination of a massive lung cancer staging project begun in 1998 by the International Association for the Study of Lung Cancer (IASLC) and will include information from large international databases that have been developed in the past decade.
The seventh edition of the guidelines will emphasize images from MDCT scanners and new survival data, and it will replace the sixth edition of guidelines (which themselves were similar to the fifth edition guidelines) that have been in place since 1997 (Chest, June 1997, Vol. 111, pp. 1710-1717).
Documented in a series of articles in the Journal of Thoracic Oncology, the proposed criteria are summarized in the IASLC's protocol documents finalized on March 27 and are available on the organization's Web site.
As the penultimate step in finalizing the guidelines, the IASLC's International Staging Committee is expected to launch a Prospective Lung Cancer Staging Project sometime this summer to validate each component of T, N, and M and other factors relevant to lung cancer staging and prognosis.
New data expressed in classifications
The reasons underlying the change are multifactorial, but they have a lot to do with survival data, said Dr. Johnny Vlahos in a presentation last week at the International Symposium on Multidetector-Row CT, sponsored by Stanford University in Stanford, CA.
The guidelines incorporate "an increase in epidemiologically detected adenocarcinoma in recent years, but also an appreciation of different patterns of disease spread -- with increased prevalence of tumors presenting with early distant metastases rather than with nodal station disease," he said (Shi et al, Journal of Thoracic Oncology, March 2006, Vol. 1:3, pp. 205-210).
The new guidelines also reflect better staging results that have been obtained from advanced imaging modalities, particularly MDCT, as well as mediastinoscopy and ultrasound-guided biopsy, said Vlahos, who is an assistant professor of radiology at New York University Langone Medical Center in New York City and a consultant radiologist at St. George's Hospital in London.
"We are now aware from surgical data that patients that we previously suspected to have a poor prognosis, such as patients with satellite nodules in the same lobe or the same lung, actually have better prognosis than we originally thought," Vlahos said (Nagai et al, Journal of Thoracic Oncology, April 2007, Vol. 2:4, pp. 282-286).
The database used to develop the new guidelines is vastly larger than the old one. While the 1997 recommendations were based on just 5,319 cases that were predominantly surgically staged, the new recommendations incorporate the findings of 100,869 cases from 46 sites in 19 countries, including 81,015 cases in which the cell type is known, with adequate initial staging information.
A total of 67,725 of the cases are non-small cell lung cancer (NSCLC). All of the cases were evaluated, at least in part, by CT, Vlahos said.
T, N, M analyzed by separate committees
Separate IASLC committees were established for the T, N, and M criteria, primarily to reclassify them according to disease survival cutpoint analysis, Vlahos explained.
For determination of staging, the criteria rely on recursive partitioning, a tree-based model for survival, and bootstrap resampling to correct the adaptive nature of the splitting algorithm. The classifications reflect a new understanding of the importance of tumor size, with recommendations for spitting tumors into several different classifications.
"There really was no effort to try to adjust the TNM classification for any problems there may have been with imaging lung cancer, but rather to adapt it to established survival data," Vlahos said.
For the T classifiers, T1 has been split into T1a (< 2 cm) and T1b (2-3 cm). Similarly, T2 has been split into T2a (3-5 cm) and T2b (5-7 cm). And the previous T2c (> 7 cm) has become a T3 designation. The aim is to refine staging based on five-year survival, Vlahos said. And according to the new data, five-year survival is pegged at 35% for the previous T2c, much closer to T3 disease (31% survival) than T2b (49%), with which it was previously classified.
Also based on survival, other proposed changes in the T classifications include:
- Satellite nodule in the same lobe as tumor: T4 to T3
- Additional nodule in ipsilateral lung, different lobe: M1 to T4
- Poor prognosis for additional nodule in contralateral lung: M1 to M1a
More information needed for nodal stage changes
"The N [nodal] descriptors have not changed," Vlahos said. "That's because exploratory analyses that were performed to try to simplify the nodal stations into six zonal areas of nodal disease did not bear up on validation across different groups in different nations, so apparently there is no recommendation to change the N descriptors, and prospective studies have been suggested."
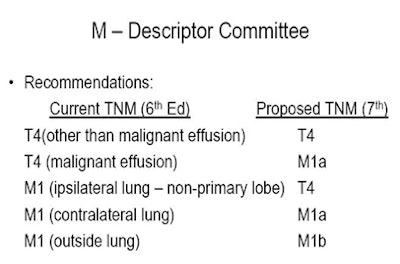
The M (metastasis) descriptors in the sixth edition, based on the nonlymphatic metastatic components of TNM (T4M0 and M1) were analyzed using Kaplan-Meier analysis of differential survival.
The results showed that "patients who have a malignant effusion with T4N0 disease have much worse [median] survival [8 months] than T4N0 patients who did not have an effusion [13 months]," Vlahos said. In addition, patients with malignant effusion had very comparable survival to those with a metastasis in the contralateral lung (10 months). However, the worst median survival (6 months) was found in patients with extrathoracic malignancy. These findings led to the following recommendations by the IASLC's M-descriptor committee:
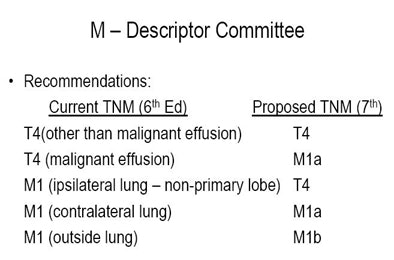 |
| Proposed M (metastasis) descriptors reflect new survival showing particularly poor prognosis for patients with pleural effusion and extrathoracic malignancies. Chart courtesy of Dr. Johnny Vlahos. |
"We must remember that M1a is intrathoracic metastatic disease, and M1b is now extrathoracic metastatic disease," he said. And among several important changes in the overall staging groupings, T4N0 and T4N1 disease that was previously IIIb disease has been migrated downward to IIIA disease.
Overall proposed seventh edition staging changes
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Proposed seventh edition overall staging changes; bolded entries indicate a change from the current sixth edition guidelines. Data from Goldstraw et al, Journal of Thoracic Oncology, August 2007, Vol. 2:8, pp. 706-714. |
Limitations
It's important to remember that the proposals are based on retrospective analysis of survival data that do not address the many limitations of current imaging and staging, Vlahos said. Nor do the proposals represent the specific tumor types that will be encountered in daily practice.
For example, bronchoalveolar cell carcinoma and multifocal bronchoalveolar cell carcinoma present a management problem that is probably worthy of a new category within the spectrum of NSCLC classifications, he said. Similarly, carcinoids and neoendocrine tumors are not specifically addressed.
"Also it doesn't really address different management pathways that we now see in our practice; for example, isolated brain or adrenal metastases that are sometimes aggressively treated are not separately categorized," Vlahos said. Nor does the system address lymphangitis carcinomatosa, or nodal deposits in unusual sites.
In addition, the classification of disease into different T and N descriptors in the new edition will result in significant stage migration, and the previous general division of IIIA (surgical) versus IIIB (nonsurgical) disease will become less definite, he said.
Vlahos and his colleagues tried out the new classifications in a study of 166 consecutive patients; they found slightly fewer cases of IIIA or lesser disease with the new system, while IIIB disease decreased significantly and stage IV disease increased substantially.
Their analysis also found:
- Migration of T4 (same-lobe nodule) to T3
- Migration of M1 (same-lung nodule) to T4
- Migration of T4 (malignant pleural disease) to M1a
- Intrathoracic M1a versus extrathoracic M1b
- Several changes of stage impacting IIIA versus IIIB
"A lot of the problems we have with the TNM classification in terms of staging remain in this current system," Vlahos said, for example, defining the size of a known central tumor. "We may be able to get some information from PET as to the size of the primary tumor, but PET is not included in the new TNM classification," he said.
There's no way to handle a situation in which it's unclear which lesion should be classified by TNM -- the peripheral lesion or the central lesion. And there is no way to handle nodes that are not within the normal descriptions, such as auxiliary nodes or abdominal nodes, Vlahos said.
By Eric Barnes
AuntMinnie.com staff writer
June 2, 2009
Related Reading
Ultrasound useful in detecting chest wall invasion by lung tumor, May 2, 2008
PET outperforms CT for diagnosis of solitary pulmonary nodules, February 18, 2008
Minimally invasive methods allow near-complete lung cancer staging, February 7, 2008
PET scans can help lung cancer diagnosis - study, November 28, 2007
PET/CT moves to prime time as first-line tool for lung cancer diagnosis, March 10, 2007
Copyright © 2009 AuntMinnie.com