BERLIN - Dual-resolution conebeam CT accentuates the positives of conebeam breast imaging and eliminates (some of) the negatives, said a team from Texas in a presentation at the Computer Assisted Radiology and Surgery (CARS) meeting.
A team from M. D. Anderson Cancer Center at the University of Texas in Houston has developed an experimental version of a CT breast imaging scanner that provides a special high-resolution region of interest within the standard conebeam breast image, a feature that gives the reader a bird's-eye view of suspicious regions of the breast for little additional radiation dose.
What does conebeam CT bring to the table that conventional mammography does not? Mammography "is intrinsically a projection technique, so it's ineffective in separating the lesions from the overlying tissue structures," said Dr. Chris Shaw from M. D. Anderson. "In recent years, tomosynthesis imaging is getting more widely used because it can better separate lesions, focusing on a thick layer of breast while avoiding outside structures."
However, because of conebeam CT's limited reconstruction angle, "it comes with artifacts that may affect the visualization of lesions," Shaw said. "And it's not a true 3D imaging technique because of the limited angle of projections available."
But conebeam CT does provide well-delineated images of breast lesions and calcifications, while avoiding the irradiation of tissues outside the organ.
Why dual-resolution breast CT?
A main limitation of traditional conebeam CT is that the technology's low exposure levels and intentionally large pixel sizes (150-400 µm) used to minimize dose can limit the visibility of microcalcifications to those larger than approximately 280 µm, Shaw said. The problem is that visualization of microcalcifications is critical for screening, diagnosis, and management of breast cancers. Without that capability, in other words, conebeam CT of the breast will remain fatally flawed.
Shaw and his colleagues aimed to circumvent this problem with a dual-resolution breast CT system that uses both a flat-panel detector and a set of high-resolution detectors to image the entire breast along with a small volume of interest (VOI), respectively.
This allows the exposure levels to be increased for the VOI selected by the operator -- potentially seeing calcium and other structures clearly -- while maintaining a reasonably low dose for the entire breast.
Full-field high-resolution breast CT remains to be developed and several groups including his are working on it, Shaw added. In a system that is similar to the new one, but without the VOI capability, the group has successfully scanned postmastectomy breasts.
While a gantry rotates around the specimen, a flat-panel detector (FPD14, Anrad, Saint-Laurent, Canada) acquires projection images of the entire breast concurrently with a high-resolution (CCD or CMOS) panel (CCD: C4742-56-I2ER, Hamamatsu Photonics, Hamamatsu, Japan) that scans a preselected 2.5-cm VOI. The low-resolution images are then combined with the VOI images and reconstructed normally, Shaw explained.
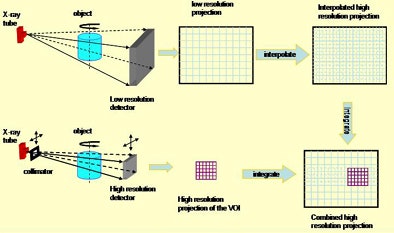 |
| With the dual-resolution conebeam CT breast imaging technique, the breast is first scanned with a low-resolution flat-panel detector at a lower exposure level to obtain conebeam CT images of the entire breast. If a suspicious region (VOI) is identified, a specially designed collimator with a circular or rectangular opening is inserted between the x-ray source and the breast. Higher-level x-ray exposure is delivered to the preselected VOI through the opening, and the projection data of the VOI are collected by a high-resolution detector. The collimator attenuates the x-ray exposure to the region outside the VOI and the scatter component in the projection image for dose reduction to the patient and better image quality. Because it is difficult to accurately reconstruct the VOI image with truncated VOI projection data only, the limit-height, full-width low-resolution projection data outside the VOI are interpolated, resampled, and used to pad the truncated space outside the VOI. Below, a photograph of the benchtop system. All images courtesy of Dr. Chris Shaw. |
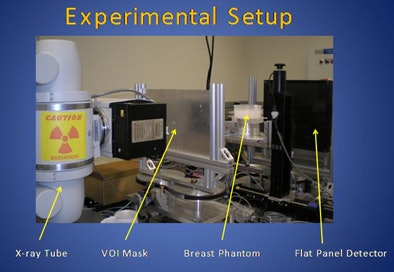 |
The researchers quantified scatter reduction using two cylindrical breast phantoms, quantifying dose savings using thermoluminescent dosimeters. For this study they scanned simulated calcifications inside wax breast phantoms. And low-contrast phantoms were scanned to simulate contrast-to-noise (C/N) ratios and figures of merit (FOMs), defined as C/N ratio2/dose to demonstrate the improvement in low-contrast performance.
The results showed that scatter-to-primary ratios inside the 2.5-cm VOI were reduced by a factor of 6.7, and by a factor of 11.6 for the small and large breast phantoms, respectively.
 |
| Nearly all of the calcifications (200-212 µm) inside the VOI were visualized. At a dose corresponding to an isocenter dose of 9 mGy, visibility of calcifications was 28%, 64%, and 64% for calcifications of 150-160 µm, 160-180 µm, and 180-200 µm. |
Meanwhile, radiation doses were reduced by a factor of 1.64 inside the VOI, a factor of 5.95 outside the VOI, and by factors of 1.89 to 7.43 for the small and large phantoms, respectively. The FOMs were improved by 117% and 209% for the small and large phantoms, respectively.
Nearly all of the calcifications (200-212 µm) inside the VOI were visualized.
"Inside the volume of interest, the scatter drops substantially," Shaw said. "Outside the VOI, there's really no change in scatter so the image quality remains affected by scatter, but we are more concerned about image quality in this [VOI] area."
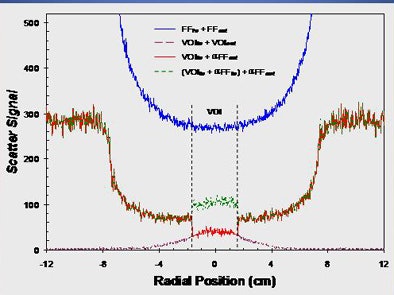 |
| Above, scatter was substantially reduced outside the VOI due to reduced direct exposure. Scatter was significantly reduced inside the VOI due to x-ray collimation (use of VOI mask). Below, scatter-to-primary (S/P) ratios were significantly reduced inside the VOI. S/P ratios remained the same outside the VOI due to full-field image acquisition. |
 |
The total exposure used for the CCD detector corresponded to an isocenter dose of 9 mGy, which is 150% of the mean glandular dose limit for two-view mammography. At this dose level, most calcifications were visible. And inside the VOI, the C/N ratio for a contrast-enhanced object improved by 15% and 29% for small and large phantoms, respectively.
 |
| Dual-resolution conebeam CT images in a 13-cm wax phantom with "calcifications" of 280-300 µm CaCO3. The dose from open-field (flat-panel) projections was 300 mR. The intentionally higher dose from VOI projections was 1.2 rads. |
"The dose is increased by a factor of six over the mean glandular dose limit [for mammography], so it's a little higher, but remember the dose is only applied to this small volume of interest, so if you calculate the overall breast dose it's pretty reasonable," Shaw said, adding that the dose and image quality parameters are also improved over standard conebeam CT.
The use of the mask reduces dose outside the VOI, and inside the ROI, as well, thanks to the extra collimation and scatter reduction. These same factors serve to decrease the radiation dose and improve both image quality and contrast, he explained.
"We demonstrated the technique with a benchtop system, and right now we're building a system for doing patient studies," Shaw said. "Because of the x-ray collimation, the scatter is reduced significantly. Because of the scatter reduction and the reduced dose outside the VOI, the breast dose can be reduced a lot. Image contrast has improved and accuracy of the CT numbers has improved."
By Eric Barnes
AuntMinnie.com staff writer
June 29, 2009
Related Reading
ECR delivers new findings on digital breast tomosynthesis, March 7, 2009
Italian study backs tomosynthesis over DR for lung pathology, February 18, 2009
New breast imaging applications show diagnostic promise, January 20, 2009
Pilot study: DBT's role needs further research, April 18, 2008
ECR sessions examine DBT's effectiveness, March 7, 2008
Copyright © 2009 AuntMinnie.com




















