An ideal pediatric chest CT exam uses low radiation dose to acquire high-quality images devoid of respiratory motion artifacts. This is easier said than done for a variety of reasons, but pediatric radiologists at a children's hospital in Ohio have figured out how to do it -- and without sedation.
CT exam quality is dependent upon the patient being able to master an unfamiliar breathing maneuver and then perform it on command. Failure to do so results in less than optimum image quality, or the need to repeat the CT scan and expose the child to more radiation dose.
The Children's Radiological Institute at Nationwide Children's Hospital in Columbus, OH, has devised a way to achieve good results almost 100% of the time. Compared to sedation, the method is simple, fast, and effective. It works for almost all children older than age 4. Even though it was developed specifically for a research study, the technique seems to be easily adoptable by any radiology department for scheduled pediatric chest CT exams.
The method uses coaching with a portable handheld spirometer that generates respiratory tracings to help children achieve targeted lung volumes. The method's key ingredients? A respiratory therapist, a spirometer connected to a laptop computer to show real-time documentation of lung volume, an empty room with a gurney, a nose clip, a small gift for the patient, and a short training session just before the scheduled procedure. The use of the process is described in an article published online in Pediatric Radiology (May 28, 2010).
Radiologists at Nationwide Children's Hospital needed to perform follow-up chest CT exams on 52 children with cystic fibrosis as part of a clinical study of lung structure and function. The study objective was to longitudinally compare baseline volume-monitored inspiratory and expiratory high-resolution CT exams and pulmonary function testing done in infancy (with sedation), using a controlled ventilation technique, with the current exams of unsedated patients.
The process
The children were as young as 4 years and as old as 13. On the day of each scheduled exam, the child first visited the CT scanning suite to become familiarized with it. Children were then taken to an adjacent room, where an experienced respiratory therapist taught them how to hold the handle of a spirometer in an inverted position, while keeping their elbows elevated and their lips tight around the spirometer's mouthpiece.
The children practiced holding the spirometer in both sitting and supine positions. When practicing the breathing exercises in a sitting position, the children were shown the display of spirometric tracings on the laptop. This enabled them to see a visual image of how they needed to breathe, and this interactive feedback presumably facilitated the training process.
The children were asked to take three tidal breaths to record a consistent end-expiratory level. The respiratory therapist then coached them to take three slow deep breaths and, on the third one, to hold the breath for approximately five seconds. They then practiced taking three deep breaths and, on the third breath, exhaling forcefully and not breathing in for five seconds. After doing this as many times as needed to master the technique, and watching the tracings on the monitor, the children repeated the exercise in a supine position.
The training sessions to master the techniques took approximately 15 to 20 minutes. The time period and success of the sessions may have been influenced by the fact that the study group had prior experience using a spirometer in a sitting position. Upon completion, the therapist and the patient promptly went to the CT suite to have the exam performed. Following this protocol minimized the potential for the patient to forget what he or she had learned and optimized scanner utilization time.
Lead author Kathryn Mueller, MD, a radiology resident at the Ohio State University College of Medicine in Columbus, and colleagues attributed the cooperation of the children to the respiratory therapist remaining next to the CT scanner to minimize their anxiety and signal the CT technologist when to perform each scan. Parents were also allowed to be in the room but were asked to remain silent.
The respiratory therapist would signal the technologist to begin the inspiratory scan on the third deep breath when a maximum volume plateau displayed on the laptop screen, and when the child's expired volume level was comparable to or lower than the previously recorded end-expiratory level for the expiratory scan. If either maneuver was not properly performed, the scan could be aborted.
For each child, a full volumetric scan was performed using 64-slice CT (LightSpeed, GE Healthcare, Chalfont St. Giles, U.K.) with age-specific dose-length product conversions. The average effective radiation dose was 0.71 mSv for inspiratory scans and 0.58 mSv for expiratory scans. The average scan duration was four seconds on inspiration and 3.6 seconds on expiration. The exam took approximately five to 10 minutes in the CT suite overall.
The results
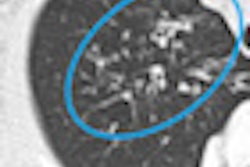
Ninety-five percent of the children reached full inflation, and all 52 inspiratory exams were obtained at a lung volume level near full inflation to optimally display the airways and parenchyma. Expiratory exams were obtained at acceptable volume levels to show any air trapping for 50 of the exams. The two patients whose images were suboptimal both were 5 years old and had substantial obstructive lung disease.
Overall, seven patients, ranging in age from 4 to 13 years, had a failure on one criteria. Two inspiratory studies and three expiratory studies revealed respiratory motion. A total of 98 out of 104 CT scans had been obtained at the correct lung volume and were free of artifacts, according to pediatric radiologist and co-author Frederick Long, MD.
The authors investigated the option of using a spirometer that electronically triggers CT scanning, but they rejected this because it had a more complex and cumbersome protocol. The use of a handheld spirometer put the patient in control of the device, which provided a comfort level to the children, allowing them to remove it to cough, swallow, or talk. This encouraged cooperation, according to the authors, along with the motivation that they would receive a present upon successfully completing the training session and the CT exam.
All children received their presents.
By Cynthia E. Keen
AuntMinnie.com staff writer
June 18, 2010
Related Reading
Pediatric CT settings should be adjusted to child's body size, May 25, 2010
Dose can be reduced by 75% in pediatric chest CT exams, June 18, 2009
Color-coded CT protocols help reduce pediatric radiation dose, June 4, 2009
Radiologists use lights, films to soothe children, December 19, 2005
Mock MRI exam preps children for the real deal, November 30, 2005
Copyright © 2010 AuntMinnie.com