
A classic duo, CT plus pulmonary function testing using spirometry, may emerge once again as a potentially effective way to diagnose lung cancer, according to an article in the July issue of Academic Radiology.
Rather than perform the standard search for pulmonary lung nodules and masses that reveal lung carcinoma, the researchers aimed to show how increased calcification at upper airway bifurcations, when combined with pulmonary function test scores, can accurately estimate an individual's risk of developing lung cancer.
To quantify the effect, they developed a quantitative method for estimating individual lung cancer risk based on analysis of airway bifurcations on high-resolution CT scans and spirometry, called the lung cancer risk index (LCRI).
The study aimed to measure the performance of the method for predicting lung cancer in patients participating in a lung cancer screening study.
"A large body of environmental health and toxicity research has demonstrated that the deposition of particulate matter is a critical mechanism governing the toxic dose exposure of the lung," wrote lead investigator Rick Avila. "Particulate matter, a major source of toxicity in cigarette smoke, is carried through the airways and deposited on the respiratory epithelium on the basis of several fundamental physical forces. This creates 'hot spots' in the lung where particulate matter deposition and exposure to noxious gasses are high" (Academic Radiology, July 2010, Vol. 17:7 pp. 830-840).
In response to smoking's continuous damage to the lungs over many years, computational fluid dynamics simulations, as well as histologic studies, have confirmed high concentrations of particulate matter in high concentrations at airway bifurcations, Avila and colleagues wrote. The studies implicate the "carinal ridge of bifurcations and the small downstream area on the surface of the airway" as regions with significant particulate matter deposition, as high as 100 times that of the tracheobronchial tree. And where there's deposition, according to the researchers, there's a high incidence of lung cancer.
The study examined 108 subjects, including 15 patients with early lung cancer (mean age, 59.7 ± 7.3 years) and 93 age-matched and pack-year-matched controls (mean age, 58.9 ± 7.2 years). The subjects were selected from an ongoing early lung cancer screening study at Clinica Universitaria de Navarra in Pamplona, Spain, that is part of an international lung cancer screening trial.
All patients with lung cancer detected in the screening study were included as long as the scan covered the lungs completely, was performed with a slice thickness of 1.25 mm or less, and had reasonable image noise, the researchers wrote. The controls, screening participants without lung cancer, were required to have smoking exposure within 10 years of a selected patient with early lung cancer.
All subjects were scanned using Somatom Definition, Sensation 64, or Volume Zoom model scanners (all from Siemens Healthcare, Erlangen, Germany) using a target-scanning protocol of tube current-time product of 40 mAs.
A subgroup of these patients underwent high-definition CT. This group included seven patients with lung cancer and 72 controls, who were scanned at 1-mm CT slice thickness.
The quantitative lung cancer risk index method is based on airway bifurcation x-ray attenuation, combined with the ratio of forced expiratory volume in one second to forced vital capacity, Avila and colleagues explained. The mean value of the five bifurcation measurements was computed.
The CT scans were measured by a single reader using the VolView image-review application (Kitware, Clifton Park, NY) using standard image-review features and using standardized window and level settings, they wrote. Lead investigator Avila has a financial interest in the method as senior director of healthcare solutions at Kitware.
The x-ray attenuation measurements were combined with spirometry by measuring forced expiratory volume in one second to forced vital capacity using a computerized spirometer (Vmax 22, SensorMedics, Yorba Linda, CA).
The spirometry test measured forced vital capacity (FVC) and forced expiratory volume (FEV1). The researchers measured the presence and severity of airflow obstruction in accordance with the criteria established by the Global Initiative for Chronic Obstructive Lung Disease.
Sensitivity was high for the detection of lung cancer using the method, and even higher for the high-resolution CT cases. A Cochran-Mantel-Haenszel analysis of the results showed a cancer detection sensitivity and specificity of 67% and 72% for all cases, and 100% and 73% for the high-resolution CT case subset.
A conditional logistic regression analysis demonstrated that a 0.0328 increase in the lung cancer risk index was associated with an odds ratio of 1.84 (95% confidence interval [CI]: 1.18-2.85) for the full dataset (p = 0.0067) and 2.89 (95% CI: 1.02-8.19) for the subset that underwent high-resolution CT (p = 0.0467).
"The odds ratios for the full dataset and the [high-resolution CT] subset provide statistically significant evidence that individuals with higher LCRIs were more likely to have lung cancer," the authors wrote.
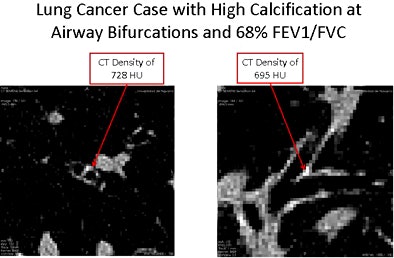 |
| Above, lung cancer patient with high levels of calcification at airway bifurcations. Case shows that high airway calcification can be observed in both small- and large-diameter airways. Images courtesy of Dr. Javier Zulueta, University of Navarra. |
To assess the relationship between lung cancer risk index and age and pack years of smoking, the group analyzed the variance testing for a linear trend between tertiles of LCRI and age multiplied by pack years in control subjects. They found a linear trend in the relationship between LCRI and tertiles of age multiplied by pack years with results that were significant at the 5% level (p for linear trend = 0.024).
The two techniques, high-resolution CT and spirometry, used to perform their technique are "two widely available and routinely used clinical tests in the management of patients," according to the authors.
The association between loss of FEV1/FVC and risk for developing lung cancer is well documented, though "the metric suffers from providing a wide risk gradient," they wrote, noting that the interrelationships between x-ray attenuation and spirometry will need to be addressed in future studies.
As for the CT measurement, "a potential explanation for increased calcification at airway bifurcations is based, at least in part, on the anatomic structure of human airway bifurcations," they noted. "The carinal ridge of a segmental airway bifurcation contains hyaline cartilage below the epithelium. Hyaline cartilage is the substrate for early bone formation and, as such, it has a natural function and propensity to calcify under numerous forms of stress."
The evidence that smoking causes the increased calcification is supported by increasing evidence that tobacco combustion products "have a profound effect in driving an exuberant and protracted immune response that can be consequential in individuals with particular genetic or epigenetic factors in which chronic inflammation may be associated with high risk for subsequent lung cancer," they wrote.
The authors concluded by stating that their method showed a statistically significant association with lung cancer, adding that the individual components of the risk model will need to be evaluated in larger cohorts to determine their validity.
"With further investigation and proper validation studies, there is the potential to provide an objective method for monitoring and managing individual lung cancer risk as well as improving our understanding of lung carcinogenesis," Avila said in a statement accompanying release of the paper. "Perhaps even more important, the approach provides a new and unexplored opportunity to better understand the fundamental biology and underlying relationships behind the development of chronic obstructive pulmonary disease and lung cancer."
By Eric Barnes
AuntMinnie.com staffs writer
June 28, 2010
Related Reading
Chest x-ray CAD offers value in detecting lung cancers, June 18, 2010
Computer-aided system increases detection of early-stage lung cancer, May 4, 2009
New CT method measures airway calcium to predict lung cancer, December 16, 2008
Dual-energy CT helps distinguish malignant lung nodules, October 8, 2008
CAD provides mixed benefits for DR lung exams, March 8, 2008
Copyright © 2010 AuntMinnie.com




















