CT can detect both the type and severity of chronic obstructive pulmonary disease (COPD), helping predict which patients will experience exacerbations, according to a new study published online in Radiology.
Researchers from the University of Michigan Health System found that quantitative measurements of lung structural changes at CT are associated with COPD flare-ups, which frequently require hospitalization. Importantly, the results were independent of spirometric measures of disease severity.
The study suggests that CT evaluation of COPD patients could be used to predict which patients are at risk of more frequent exacerbations, helping direct a range of targeted therapies.
"Spirometry is inadequate as the sole parameter for assessing risk of exacerbations," lead author Dr. Meilan Han said in a statement accompanying the study's release. "Two COPD patients may be identical in terms of lung function yet behave very differently. For instance, there are subsets of patients with severely reduced lung function who do not experience frequent exacerbations."
COPD can damage the bronchi as well as the lung alveoli and is a leading cause of death and illness worldwide, the group explained. The two main structural abnormalities seen in COPD are emphysema, in which the alveoli are gradually destroyed, and airway disease, which causes a narrowing of the bronchial tubes.
Han and her team aimed to test the hypothesis that a relationship exists between COPD exacerbation frequency and quantitative CT measures of emphysema and airway disease.
Quantitative metrics at CT are becoming increasingly important for evaluating diseases related to smoking, the group wrote. The association between CT measurements of severity and disease phenotypes has been explored previously, but not in a large population with diverse disease types.
Flare-ups are expensive. Most of the nearly $50 billion spent to treat COPD in the U.S. last year was directed toward the treatment of exacerbations, particularly patients requiring hospitalization for their symptoms, the authors wrote.
"Being able to predict which patients are at the greatest risk for acute COPD exacerbations will enable health care providers to better target these individuals for preventive therapy," wrote Han, Dr. Ella Kazerooni, Dr. David Lynch, and colleagues (Radiology, July 25, 2011).
The study examined 2,500 patients (mean age, 64.7 years ± 8.5 years; 54% men; mean 51.5 ± 21.5 pack-years of smoking) who were also participants in the COPDGene study. Participants were scanned using an inspiratory/expiratory COPD protocol on 16- and 64-detector-row scanners (LightSpeed and VCT, GE Healthcare) at 0.625-mm collimation, 100 and 400 mAs, and 120 kVp.
The authors measured total lung emphysema percentage by using an attenuation mask technique. Total emphysema percentage was defined as all lung voxels with a CT attenuation value of less than -950 HU.
Software was used to measure mean wall thickness and mean wall area percentage in six segmental bronchi. Finally, a questionnaire was used to learn about COPD exacerbations during the previous year, and statistical analysis was performed to examine the relationship of exacerbation frequency with lung function and quantitative CT measurements.
In a multivariate analysis adjusted for lung function, the results showed that bronchial wall thickness and total lung emphysema percentage were associated with COPD exacerbation frequency. Each 1-mm increase in bronchial wall thickness was associated with a 1.84-fold increase in annual exacerbation rate (p = 0.004).
In addition, while many patients had a mixture of structural changes related to their COPD, two subgroups predominantly with emphysema or large airway disease could be identified.
Patients with more than 35% emphysema volume and wall thickness greater than 1.75 mm had a higher COPD exacerbation frequency than did the subjects with less than 35% emphysema and a wall thickness of less than 1.75 mm.
The less-severe patients in both groups reported experiencing a mean of 0.62 exacerbation per year, compared with means of 1.1 exacerbations per year reported by the emphysema-predominant group (p < 0.0001) and 0.8 exacerbation per year reported by the airway-predominant group (p = 0.07).
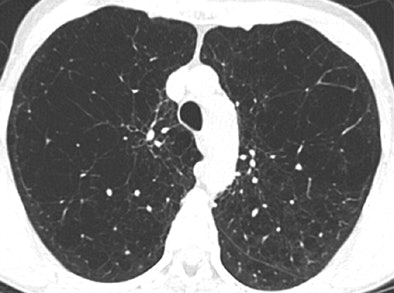 |
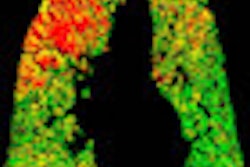
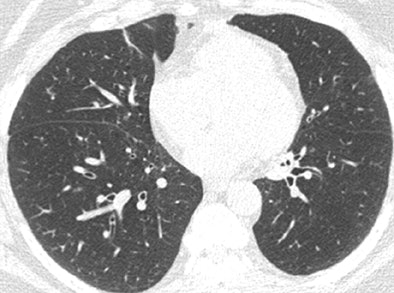
| Axial CT scans in two subjects with different COPD phenotypes: emphysema-predominant COPD (≥ 35% emphysema, <1.75-mm segmental bronchial wall thickness) (above) and airway-predominant COPD (<35% emphysema, ≥ 1.75-mm segmental bronchial wall thickness) (below). Images republished with permission of the Radiological Society of North America, from Radiology, July 25, 2011, 110173. |
 |
The results are in line with preliminary studies, and support the use of radiologic phenotyping with use of whole-lung volumetric high-spatial-resolution CT. In addition, the results were independent of spirometric measures of lung function, the authors noted.
"Airway inflammation, as measured by using wall thickness at the segmental level, offers additional potentially important prognostic information beyond that assessed with spirometry alone," Han and colleagues wrote. "Wall thickness may be the macroscopic correlate of mucus gland hypertrophy and airway inflammation, which plausibly relate to infection, the principal cause of COPD exacerbations. These data, however, cannot be used to determine whether bronchial wall thickness is simply the effect of the previous exacerbations or predates them and thus possibly has a causal role."
Another important finding was the nonlinear relationship observed between emphysema percentage and exacerbation frequency, demonstrating that exacerbation frequency "is related to both emphysema severity and airway disease," the authors wrote.
"Radiologic characterization of COPD patients has prognostic value in the selection of more homogeneous subgroups for clinical trials and possibly for identifying patients at risk of frequent exacerbations for targeted medical therapies," Han said in her statement.