CT data from virtual colonoscopy studies are ideal for assessing bone mineral density (BMD), say researchers from the University of Wisconsin in Madison. They found that virtual colonoscopy data from the lumbar spine showed excellent correlation with bone density's gold standard, dual-energy x-ray absorptiometry (DEXA).
The accuracy of the results remained high whether BMD was measured using quantitative CT (QCT) or by means of a simple region of interest (ROI) CT density assessment. This means that virtual colonoscopy (also known as CT colonography or CTC) alone can effectively rule out osteoporosis and osteopenia without need of a second test such as DEXA, according to the study team.
"As we know, osteoporosis is a major public health concern, with up to half of all women and even 20% of men having a lifetime risk for osteoporosis-related fracture," said Perry Pickhardt, MD, in a presentation at the International Symposium on Virtual Colonoscopy in October. "DEXA bone mineral density screening is the gold standard, but it is underutilized."
Offering a two-for-one screening study could boost compliance for people at risk of both colorectal cancer and osteoporosis, potentially improving health outcomes for screening patients, Pickhardt said.
Adding osteoporosis screening to VC "can efficiently determine who is at risk for osteoporosis and who is not," Pickhardt told AuntMinnie.com. "This information at CT is currently being wasted. Obtaining a simple, single-level [e.g., L1] ROI measurement of vertebral body trabecular attenuation takes a matter of seconds" and adds value to the CTC exam in the same way abdominal aortic aneurysm screening can be performed with the same CT data.
The study used both quantitative CT and simple trabecular ROI attenuation approaches to bone density measurement, with DEXA serving as the reference standard. DEXA isn't a perfect gold standard -- "in fact, we believe CT is more accurate," Pickhardt said. But because DEXA T-scores are the standard used by "all the major national and international societies," including the World Health Organization, "we have to use DEXA whether we like it or not," Pickhardt said. "It's analogous to [performing] CTC and using colonoscopy as the reference standard."
Pickhardt and colleagues including Lawrence Lee, MD, and Alejandro Muñoz del Rio sought to evaluate the performance of lumbar spine BMD assessment at screening CTC. Secondary aims of the study included assessment of supine versus prone measurements for both QCT and simple ROI methods. The investigators were also looking to detect unsuspected lumbar compression factors at CTC, which DEXA can miss, compare 1.5-mm and 5-mm reconstruction thicknesses, and evaluate interobserver variability.
DEXA can produce false-negative results for osteoporosis in the setting of unsuspected lumbar compression fractures that CT can potentially detect, according to Pickhardt.
The study included 252 adults (240 women, 12 men; mean age, 58.9 years) who underwent both DEXA and CTC screening within three months of each other (mean interval, 19.7 days; range, 1-60) between 2004 and 2008. Central DEXA was performed on a Lunar Prodigy (GE Healthcare, Chalfont St. Giles, U.K.) according to established guidelines, with measurements based on the lowest DEXA T-score between the spine and the hip.
Osteoporosis, defined as a T-score of -2.5 or less at DEXA, was found in 29 of 252 patients (11.5% prevalence). Osteopenia, defined as a T-score between -1.0 and -2.4, was found in 139 of 252 patients (55.2%).
Virtual colonoscopy was performed on scanners ranging from 8 to 64 detector rows (GE Healthcare) in the normal manner following automated insufflation of the colon (ProtoCO2l, Bracco Diagnostics, Princeton, NJ) and cathartic bowel cleansing (30-300 mA, 120 kVp, 1.25-mm collimation, and 1.25- and 5-mm slice thickness).
The team applied phantomless QCT software as well as nonangled trabecular measurements to the T12 to L5 levels on all supine VC series, and accuracy was assessed using univariate and multivariate ROC curves and threshold analyses.
The study group recorded the actual bone mineral density value in grams per cubic centimeter instead of using the T-scores or the Z-scores produced by the phantomless QCT software "because they don't really have a reference standard that's accepted," Pickhardt said. The "simple ROI" technique was performed without angulation or precise measurements.
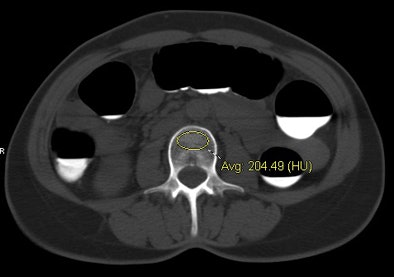 |
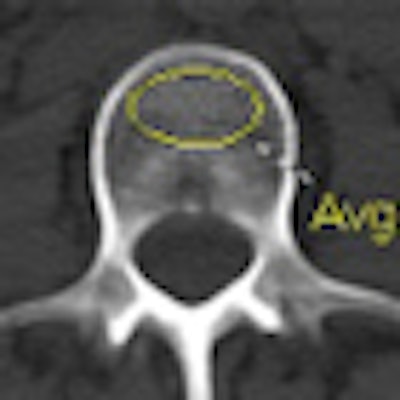
| CT data from virtual colonoscopy exam shows individual with normal BMD (top) and another with osteoporosis (bottom). Both cases were assessed at the L3 level using the simple ROI method, with results confirmed by DEXA. Images courtesy of Perry Pickhardt, MD. |
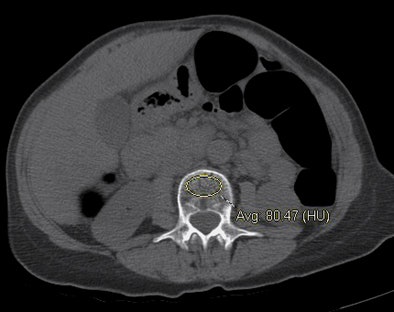 |
"We simply lay an ovoid ROI and measure the mean attenuation in Hounsfield units," he said. Reconstructions were performed at both 1.5-mm and 5-mm thicknesses and the two were compared -- but the focus was on 5-mm thicknesses because they are compatible with any routine CT study.
The group reviewed sagittal reconstructions for vertebral deformities such as compression fractures using the Genant visual semiquantitative scale. Finally, the researchers evaluated the measurement precision of both QCT and the ROI method using Bland-Altman plots on a subset of 45 cases using both supine and prone VC series.
The analysis showed similar results across the board -- with no significant differences for any of the measurements versus DEXA, Pickhardt said.
"In the ROC analysis, the area under the curve [AUC] was actually quite good for QCT and for the simple ROI method," he said. "The 95% confidence interval levels overlapped broadly for all [measurement methods], so they're quite similar."
At quantitative CT, a BMD threshold of 90 g/cm3 yielded 100% sensitivity for osteoporosis (29/29). Seventy (83.3%) of 84 adults with normal BMD were above this threshold and 99 (87.6%) were below it.
"If we find a threshold that makes the technique 100% sensitive for osteoporosis -- at QCT that would be a level of 90 g/cm3 -- we achieve 100% sensitivity because that's what we're going for, but all of the patients below the threshold will have a low BMD for either osteoporosis or osteopenia, and about half of the patients above that threshold will have a normal bone density or at worst osteopenia, which is of questionable clinical relevance," Pickhardt said.
For example, at the L3 level, a trabecular attenuation threshold of 130 HU was 100% sensitive for osteoporosis (29/29); 61 (72.6%) of 84 adults with normal BMD were above the 130 HU threshold, while 108 (82.4%) of 131 below 130 HU had osteopenia or osteoporosis at DEXA. Similar results were found for other T12-L5 levels; complete results are shown below.
AUC for osteoporosis (no significant differences between any of the measurement methods):
- QCT: 0.865 (0.755-0.930)
- Simple ROI T12-L5: 0.826 (0.712-0.902)
- Simple ROI multivariate analysis: 0.828 (0.714-0.902)
- Simple ROI L3: 0.815 (0.701-0.893)
AUC for low bone mineral density (osteopenia + osteoporosis):
- QCT: 0.778 (0.717-0.830)
- Simple ROI T12-L5: 0.793 (0.733-0.842)
- Simple ROI L1: 0.789 (0.729-0.838)
QCT BMD at a threshold of 90 g/cm3:
- 100% (29/29) sensitivity for osteoporosis
- 86.7% (98/113) less than 90 g/cm3 had low BMD
- 49.6% (69/139) greater than 90 g/cm3 had normal BMD
Simple L3 trabecular threshold of 130 HU:
- 100% (29/29) sensitivity for osteoporosis
- 82.4% (108/131) less than 130 HU had low BMD
- 72.6% (61/84) greater than 130 HU had normal BMD
Supine-prone measurement precision was slightly more accurate for the VC method than QCT, probably owing to differences in the measurement of muscle and subcutaneous fat, which varied substantially from patient to patient, Pickhardt said.
"At CTC screening both lumbar QCT and simple ROI measurements are effective at assessing bone mineral density relative to DEXA, which is a reference standard we have to use," he said. "We can set a certain level and be at 100% sensitivity for osteoporosis and also exclude osteoporosis in a large fraction of people -- over half of people depending on the level -- and actually preclude the need, possibly, for DEXA in those cases."
By Eric Barnes
AuntMinnie.com staff writer
January 20, 2011
Related Reading
DEXA advised for kids at risk of bone disorders: AAP guidelines, January 7, 2011
QCT identifies bone loss after ob/gyn cancer treatment, November 26, 2010
Automated QCT offers hope for passive osteoporosis screening, December 28, 2009
MDCT holds promise for advanced osteoporosis scan, April 6, 2009
UCSF adds bone mineral density test to VC colon screening, December 3, 2008
Copyright © 2011 AuntMinnie.com