Data from CT colonography (CTC) scans can be used for a comprehensive assessment of bone strength and bone mineral density, according to the results of a study in Radiology. The new technology goes beyond what's provided by dual-energy x-ray absorptiometry (DEXA) and could improve clinicians' ability to assess fracture risk.
The study from the Mayo Clinic in Rochester, MN, compared the use of biomechanical CT analysis and conventional DEXA for diagnosing osteoporosis and assessing fracture risk in 136 women. The results revealed high sensitivity for noninvasive biochemical CT analysis versus DEXA, and it was even more accurate than previous CT osteoporosis analysis techniques.
The retrospective analysis of CT colonography data offers comprehensive osteoporosis assessment, the authors wrote (Radiology, July 22, 2015).
"This is another study that shows the potential useful ancillary information that can be obtained from CTC and CT scans in general by using dedicated software," lead author Dr. Jeff Fidler wrote in an email to AuntMinnie.com. "This study used unique engineering software (similar to what is used in assessing bridge strength) that provides information regarding bone strength in addition to bone density, which has not been previously performed on CTC data."
Barriers to osteoporosis screening
Despite the aging population in the U.S., most people are never screened for osteoporosis. Low reimbursement for DEXA may be a factor, as well as the need for a separate test, according to the authors.
Previous approaches have used CT to identify patients who should be recommended for DEXA screening, but the current study uses a more comprehensive test. The study group's biomechanical CT analysis provides DEXA-equivalent measurements of bone mineral density (BMD) and T-scores at the hip and of vertebral trabecular BMD at the spine "to directly identify patients with osteoporosis who are at high risk for fracture," Fidler and colleagues wrote.
The researchers retrospectively analyzed data from CTC studies performed between January 2008 and April 2010 in 136 women (age, 43-92 years). All of the subjects had undergone hip DEXA within six months of the CTC exam.
The CTC exams were acquired on a 16-detector-row scanner (LightSpeed Pro 16, GE Healthcare) using 120 kVp and patient-size-adjusted tube current set at a mean of 64.1 mAs (range, 27-168 mAs).
Under the hood
Each CTC image was calibrated to convert CT attenuation values into units of BMD via an existing phantomless approach that used air, fat, and/or blood as an internal reference for each patient individually. Additional processing on the left hip was also performed when possible. The DEXA-based classifications were then compared against the biomechanical CT classifications, largely based on T-scores, which measure bone mineral density.
The biomechanical CT analysis results and DEXA readings were highly correlated for T-scores at the femoral neck (R2 = 0.84), and the mean difference in T-score units between the two techniques was not statistically significant (p = 0.15).
Using DEXA as the reference standard, CT had 100% sensitivity in eight of eight patients and 98.4% specificity in 126 of 128 patients for identifying osteoporosis at the femoral neck, according to Fidler and colleagues.
When the hip and spine were also included, the classification of patients at high risk for fracture by biomechanical CT analysis (those with osteoporosis or low bone strength) strongly agreed with the classification of clinical osteoporosis by DEXA, with 82.8% sensitivity in 24 of 29 subjects and 85.7% specificity in 66 of 77.
"The results showed good correlation with DEXA, but also provided additional information regarding bone strength and identified patients with weak bones that may not demonstrate osteoporosis-level bone density measurements," Fidler told AuntMinnie.com.
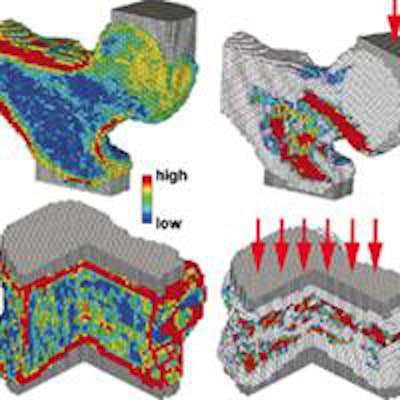
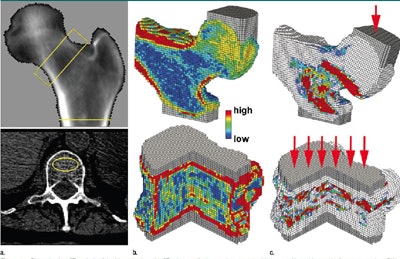 78-year-old woman with positive results for osteoporosis and fragile bone strength at the hip and spine. (a) DEXA-equivalent BMD analysis of the virtually isolated proximal femur (top) shows the femoral neck and total hip regions of interest, and quantitative BMD analysis of the L1 vertebral trabecular bone (bottom) shows the elliptical region of interest. (b) Cutout views show the distribution of bone material properties as derived from CT attenuation data. (c) Virtual deformation patterns show regions of simulated bone tissue failure. White = unfailed tissue; red = most extensive failure. Images published with permission from RSNA.
78-year-old woman with positive results for osteoporosis and fragile bone strength at the hip and spine. (a) DEXA-equivalent BMD analysis of the virtually isolated proximal femur (top) shows the femoral neck and total hip regions of interest, and quantitative BMD analysis of the L1 vertebral trabecular bone (bottom) shows the elliptical region of interest. (b) Cutout views show the distribution of bone material properties as derived from CT attenuation data. (c) Virtual deformation patterns show regions of simulated bone tissue failure. White = unfailed tissue; red = most extensive failure. Images published with permission from RSNA.Study limitations
Regarding limitations of the research, the gold standard that biomechanical CT analysis was compared to -- DEXA BMD -- is influenced by aortic mineralization and other common degenerative changes, the authors noted.
"Such differences may explain why the risk for vertebral fracture is more highly associated with CT-based measures of vertebral trabecular BMD than it is with [DEXA]-based measures of spinal BMD," they wrote.
"This technology can potentially identify patients at risk for fracture who otherwise wouldn't have been identified by just assessing bone density," Fidler wrote in his email.
Ultimately it is clinicians, endocrinologists, and medical societies who will decide how and if the technology is used clinically, Fidler said. More education is needed to help clinicians become more comfortable making treatment decisions based on bone CT results.
"The ideal situation would be that DEXA would not be required, but until there is more widespread understanding and implementation of this technique by societies, clinicians may still feel the need to order subsequent DEXA to be used in follow-up," Fidler said.
New guidelines from the International Society for Clinical Densitometry (ISCD) have confirmed CT-generated bone strength and BMD measurements as a basis for treatment, and radiologists can help with interpretation, he said.
The researchers have begun rolling out the technology in their own institution.




















