Combining math-based models with 3D dual-energy x-ray absorptiometry (DEXA) models of the femur enabled clinicians to predict an individual's risk of hip fracture with an accuracy greater than that of standard DEXA and comparable to CT, according to an article published in the April issue of Bone.
The researchers, led by first author Carlos Wills, PhD, from Pompeu Fabra University in Barcelona, Spain, developed a technique for predicting hip fracture risk by analyzing 3D models based on conventional DEXA exams and math equations. They found that their technique predicted hip fracture risk in individuals with osteoporosis with an accuracy of up to 0.91, depending on the location of the fracture (Bone, April 2019, Vol. 121, pp. 89-99).
"The modeling and biomechanical simulation of the bone by means of finite element-based 3D reconstructions of conventional bone densitometry [DEXA] provide descriptors of the internal tissue mechanics that go beyond the traditionally explored bone density when it comes to discriminating the risk of osteoporotic fracture," Wills said in a statement from the university.
3D DEXA
The long-held gold standard for identifying individuals with osteoporosis and estimating their risk of fracture has been to calculate bone mineral density on DEXA scans. A major limitation of conventional DEXA is that its 2D measurements do not provide information on the 3D spatial distribution of bone mineral density.
As an alternative to DEXA, clinicians have used volumetric bone mineral density measurements from quantitative CT (QCT) to predict an individual's risk of fracture, the authors noted. Various groups have reported a better predictive ability with QCT, but at the cost of increased radiation dose and a greater financial burden.
To address these limitations, Wills and colleagues explored the possibility of using 3D DEXA measurements to predict fracture risk. To that end, they acquired data from 111 individuals who had previously undergone a DEXA exam of the femur for suspicion of osteoporosis. The average age of the individuals was 56.2 years, and 73% were women.
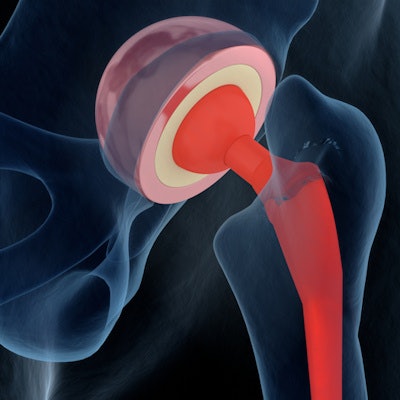
The researchers used computer software (3D-Shaper v2.6, Galgo Medical) to convert the standard DEXA scans into patient-specific 3D virtual models and then obtain volumetric bone mineral density measurements. Next, they combined these 3D DEXA models with generic 3D femur models that they generated using the finite element method, a math technique that employs algebraic equations to create models.
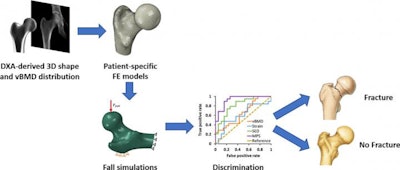 3D DEXA workflow. Image courtesy of Pompeu Fabra University.
3D DEXA workflow. Image courtesy of Pompeu Fabra University.By combining the finite element and 3D DEXA models, the team was able to simulate a typical falling scenario for each of the 111 cases examined, as well as determine the likely effect that falling down would have on an individual's upper thigh bones. The quantitative data drawn from the simulation, in turn, allowed researchers to predict each individual's risk of hip fracture after a fall.
"The simulations obtained by this research include three-dimensional interaction between bone density, the geometry of the femur, and external mechanical loads, which cannot be measured in a patient [using conventional techniques alone]," co-author Dr. Luis Miguel del Rio, a radiologist from CETIR Medical Group said.
Better predictor
The researchers focused their evaluation of the 3D DEXA and finite element models on the two most common points of femur fracture: the neck zone, which supports the head of the femur, and the trochanter zone just below the neck region. Their analysis of the bone mineral density measurements taken from the 3D models allowed for a more accurate prediction of hip fracture risk than estimates obtained using standard DEXA scores alone.
To be specific, one of the key measurements of the 3D models -- major principal stress -- had an area under the curve (AUC) of 0.81 for predicting fractures in the neck zone of the femur, and an AUC of 0.91 in the trochanter zone. These values demonstrate a marked improvement in prediction accuracy compared with the maximum AUC of 0.7 for conventional DEXA reported in current literature.
| Risk prediction for hip fracture in individuals with osteoporosis | |||||
| DEXA | Quantitative CT | 3D DEXA + 3D math models | |||
| Neck of femur | Trochanter of femur | Neck of femur | Trochanter of femur | ||
| AUC | ≤ 0.7* | 0.94* | 0.79* | 0.81 | 0.91 |
The data not only highlighted the improved risk prediction capabilities of 3D DEXA but also revealed that the trochanter region's capacity to withstand stress may be one of the most critical factors to consider when evaluating fracture risk, according to the authors.
"Advanced image analysis provides a customized framework of modeling and augmented reality, by integrating the morphology and the densities of the patients' bones into virtual models," senior author Jérôme Noailly, PhD, said. "Moreover, the conversion of these models into finite element models capable of integrating equations of the bone's mechanical behavior in the event of external mechanical events, such as a fall, enables calculating descriptors that uniquely integrate crossed effects between bone quality, particular bone morphology, and external mechanical forces."